Although studies have shown that African-American men present with significantly more advanced prostate cancer than white Americans, race has no bearing on the outcome of treatment with permanent prostate brachytherapy. That’s the conclusion reached by a group of researchers from New York City in a study published in the International Journal of Radiation Oncology, Biology and Physics.
Dr. Lucille Lee from Memorial Sloan-Kettering Cancer Center and colleagues tracked 1,081 consecutive patients who underwent permanent prostate brachytherapy, including 246 African-Americans, to compare prostate-specific antigen relapse-free survival (PSA-RFS) in both populations. Lee’s co-authors were Dr. Taryn Torre and Dr. Louis Potters from Memorial Sloan-Kettering and Dr. Carlton Barnswell and Michael Kattan, Ph.D., from Mercy Medical Center in New York City.
All of the patients had biopsy-proven adenocarcinoma and were staged according to the standards of the American Joint Committee on Cancer. All patients underwent transrectal ultrasound (TRUS) to assess prostate size. Those with glands greater than 60 cc received 3-4 months of hormone therapy consisting of a luteinizing hormone-releasing hormone (LHRH) agonist, with or without an anti-androgen.
The patients underwent permanent prostate brachytherapy with 144 Gy iodine-125 or 140 Gy palladium-103. If electron beam radiation therapy (EBRT) was added, then the dose was lowered to 110 Gy for 125I and 105 Gy for 103Pd.
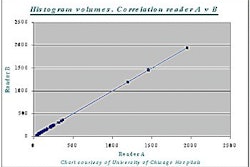
Follow-up was done at five weeks, then every 3-4 months for 2 years, and then every 6 months thereafter. At each visit, a serum PSA level was drawn. Follow-up PSA values were entered into a database, which offered information on PSA failure across the entire cohort. A modified version of the American Society for Therapeutic Radiology and Oncology’s definition of PSA-RFS was applied.
"This definition marks failure at the midpoint in time between the post-treatment nadir and the first of three consecutive PSA rises. The requirement that the three rises be consecutive was relaxed. For patients whose most recent PSA values were rising at the time of their last follow-up, but in whom failure had not occurred, follow-up time was truncated at the PSA immediately before the first rise," the authors explained (International Journal of Radiation Oncology, Biology and Physics, June 2002, Vol.53:2, pp. 282-289).
According to an analysis of the entire cohort, the 5-year PSA-RFS was 81.9%. Based on a multivariate analysis, the PSA-RFS was 84% for African-Americans and 79.4% for white Americans. Thus, race was not a significant prognostic factor.
However, there were some differences in treatment and disease characteristics. More African-American men, 41.5%, received neoadjuvant androgen ablation (NAAD) compared to 27.2% of the white patients. The African-American patients were younger (66.9 years versus 69.5 years) at presentation. They also had a lower disease stage and a lower Gleason score, the group reported.
For the matched-pair analysis, 246 patients were pulled from each group, based on neoadjuvant hormone administration, Gleason score, and pretreatment PSA value. Again, no significant differences were observed, with the 5-year PSA-RFS for African-American patients at 84% and 81.2% for white patients.
"Despite (previous) observations that African-American patients in the general population present with more advanced disease, freedom from failure seems to be the same when known pretreatment prognostic factors are controlled," the authors stated.
By Shalmali PalAuntMinnie.com staff writer
July 10, 2002
Related Reading
Lack of screening does not explain breast cancer stage variations in minorities, July 5, 2002
Socioeconomic status effects US breast cancer care more than race, April 4, 2002
Breast cancer risk often misinterpreted, March 30, 2001
Copyright © 2002 AuntMinnie.com