Looking to keep your prostate performing at its peak? Then pop a few peppers in your mouth, according to a new study that found capsaicin causes prostate cancer cells to self-destruct.
In an animal study conducted by hematologists and radiation oncologists from the U.S. and Japan, capsaicin -- the ingredient that gives chili peppers their kick -- had a "profound antiproliferative effect on prostate cancer cells, inducing the apoptosis of both androgen receptor-positive and (receptor)-negative prostate cancer cell lines." In mice that were fed capsaicin, tumors were one-fifth the size of tumors in untreated mice (Cancer Research, March 15, 2006, Vol. 66:6, pp. 3222-3229).
One of the authors, Dr. Sören Lehmann from Cedars-Sinai Medical Center and the University of California, Los Angeles, estimated that the mice consumed 400 mg of capsaicin three times a week, which is the equivalent of three to eight fresh habañero peppers, depending on their degree of heat (Reuters Health, March 15, 2006).
Of course, pepper consumption won't exempt you from the need for prostate screening with a prostate-specific antigen (PSA) exam and digital rectal exam (DRE). The American Urological Association and the American Cancer Society advise yearly PSA and DRE screening, starting at age 50. Screening should start 10 years earlier if there is a family history or the patient is African American.
Another study showed that PSA testing is an accurate exam that has not resulted in overdiagnosis of prostate cancer. Urologists from Northwestern University in Chicago and Washington University in St. Louis looked at the pathological characteristics of screening-detected cancers.
Over a 12-year period, more than 35,000 men were enrolled in a longitudinal prostate cancer screening study. The authors evaluated data from the 10% of men ultimately diagnosed with prostate cancer. They found that 99.8% of the cases were clinically localized.
Also, less than 10% of tumors would have been considered clinically insignificant based on previously published pathological criteria. The group concluded that PSA testing resulted in a lower detection rate and that the majority of cancers met the pathological criteria for significance (Journal of Urology, March 2006, Vol. 175:3, Pt. 1, pp. 902-906).
So PSA testing has value as a screening tool, but what is as effective for gauging treatment for prostate carcinoma? A multi-institutional group conducted a study to determine the significance of PSA nadir (nPSA) and time to nPSA (TnPSA) for predicting cancer recurrence in patients treated with external-beam radiation therapy (EBRT).
"After primary radiotherapy, residual benign and malignant prostate tissues continue to produce detectable PSA in most cases," wrote Dr. Michael Ray, Ph.D., and colleagues. "The findings from this study have confirmed the importance of PSA level after RT as a powerful predictor of prostate cancer outcomes" (International Journal of Radiation, Biology, Physics, March 2006, Vol. 64:4, pp. 1140-1150).
Ray is from the University of Michigan in Ann Arbor. His co-authors are from various institutions in Houston; Philadelphia; Cleveland; St. Louis; Boston; New York City; Royal Oak, MI; and Rochester, MN.
For this study, 4,833 patients met the criteria for analysis. The median follow-up time was 6.3 years. At five years, 2,049 patients were still available for analysis and 616 were available at eight years. All patients were treated with EBRT alone to doses equal to or greater than 60 Gy without neoadjuvant or adjuvant androgen suppression. The two end points for this study were PSA disease-free survival (PSA-DFS) and distant metastasis-free survival (DMFS).
The results showed that a lower nPSA level was significantly associated with improved PSA-DFS. In addition, a longer TnPSA was significantly associated with improved PSA-DFS. Finally, a lower nPSA level was tied to improvement in the purely clinical end point of DMFS, the authors stated.
For low-risk patients (nPSA of 0-0.49 ng/mL), the eight-year PSA-DFS rate was 81% and the DMFS was 100%. Patients in the intermediate-risk group had an eight-year PSA-DFS rate of 73% and a DMFS rate of 97%. For high-risk patients, the eight-year PSA-DFS was 66% and the DMFS was 92%.
"In this analysis, cut points of six, 12, and 24 months between RT completion and nPSA were selected, and significant associations between a longer TnPSA and improved biochemical and distant failure-free survival were found," the authors stated. "A rapid nadir may reflect a more immediate effect of RT against malignant tissue, and further decreases in nadir at later intervals may reflect more prolonged effects on normal prostatic tissue."
Ray's group cautioned that while nPSA proved to be a useful prognostic factor in this study, a single nPSA cut point cannot be relied upon to determine if treatment was successful. Rather, these predictive, biochemical markers can help identify higher-risk patients who would benefit from early adjuvant or salvage therapies.
By Shalmali Pal
AuntMinnie.com staff writer
April 17, 2006
Pepper image courtesy of www.classroomclipart.com.
Related Reading
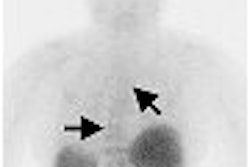
F-18 fluoride PET/CT accurately detects bone metastases in high-risk prostate cancer, March 10, 2006
Brachytherapy, high-dose radiation both effective for early prostate cancer, February 28, 2006
Prostate re-screening interval could be safely extended for some, February 23, 2006
Guide aims to help men understand prostate cancer, September 12, 2005
Urologist promotes brachytherapy for prostate cancer, May 3, 2005
Copyright © 2006 AuntMinnie.com