Preclinical studies suggest that anti-angiogenic drugs will have the greatest effect when used in tandem with chemotherapy and/or radiotherapy. The question is: How can these elements combine into the most effective treatment regime? Dosages, treatment timescales, and the order that different therapies are administered will all have an impact on overall efficacy. Until this puzzle is solved, the potential of anti-angiogenic drugs may not be fully realized.
"There has been some great success applying anti-angiogenic therapies to mouse models. But really there isn't a clear strategy on how you should use cytotoxic therapies in combination with anti-angiogenics, where radiotherapy would fit in, and whether there is some way of optimizing these treatment strategies," said Siv Sivaloganathan, Ph.D., a professor of applied mathematics at the University of Waterloo in Ontario and director of the Fields Institute Centre for Mathematical Medicine in Toronto.
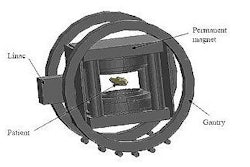
This complex scenario has now been distilled into a single mathematical model that promises to help oncologists with their clinical decision-making. Assistant professor Mohammad Kohandel and colleagues used a reaction-diffusion equation to study the spatial and temporal arrangement of cells in a growing tumor. A simple coarse-grained model producing islands of vascular and nonvascular networks was used to describe the process of angiogenesis. A third equation accounted for the concentration of oxygen, or other nutrients, available to the growing tumor (Physics in Medicine and Biology, July 2007, Vol. 52:13, pp. 3665-3677).
Team members then used the model to examine the effects of single and combined administration of radiotherapy and anti-angiogenic therapy. Their simulations matched closely with experimental results that had indicated anti-angiogenic drugs are most effective at slowing tumor growth when administered prior to radiotherapy. The model also showed the effect of combined treatments on the tumor's vital oxygen supply. A study of chemotherapeutic drugs, using the same model, is forthcoming.
Spotting the links
The mechanisms of cancer growth and therapy response are undoubtedly complex, and linking events that are happening at the cellular level with effects at tissue level is a real challenge, said Sivaloganathan, who co-authored the work. He cited close collaboration with oncologists as a key factor in the model's clinical relevance.
"Our feeling right from the beginning has been that the medical problem has to drive the math," he said. "By talking to physicians and medical scientists, you can postulate whether one mechanism might be crucial and another less important, and then you can incorporate these into your mathematical modeling."
Such models may, in the future, help oncologists optimize regimes for treating different cancers. Physiological data from patients could even be used to plan individualized therapeutic approaches. Software capable of personalizing medicine in this manner is likely to be available within five to 10 years, Sivaloganathan told Medicalphysicsweb.
Clinicians and experimental scientists led by Mike Milosevic at the Princess Margaret Hospital in Toronto will now be assessing the model's predictive prowess in mice. Clinical trials may follow, depending on the accuracy of the mathematical simulations.
In the meantime, Kohandel and Sivaloganathan, in collaboration with Mehran Kardar, a professor of physics at the Massachusetts Institute of Technology in Cambridge, MA, are continuing to refine their model to take account of the latest biomedical research.
For example, the model currently presumes that killing any cell within the tumor will have the same effect. More recent studies now suggest that a small proportion of cancer cells are responsible for driving tumor growth. Targeting this subpopulation of cells will consequently have a greater impact on treatment efficacy.
"This hasn't been proven, but there is more and more evidence emerging. So we are trying to incorporate this hypothesis into our model as well," Sivaloganathan said.
By Paula Gould
Medicalphysicsweb contributing editor
September 14, 2007
Related Reading
Blocking angiogenesis may render tumors radiosensitive, June 21, 2007
Urokinase expression inhibits tumor progression, June 12, 2006
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community Web site covering fundamental research and emerging technologies in medical imaging and radiation therapy.