Children diagnosed with medulloblastoma have an excellent chance of being cured. Unfortunately, the treatment needed to survive can be bittersweet, because many young patients face a risk of hearing loss from the combined ototoxicity of cisplatin-based chemotherapy and radiation therapy.
A research study published in 2002 offered some hope for pediatric medulloblastoma patients, finding that intensity-modulated radiation therapy (IMRT) could dramatically reduce severe ototoxicity. But the study had several shortcomings, including a small sample size of 15 patients, a short median follow-up period of only 18 months, and a potential radiation underdosage to the patients who received IMRT, according to Dr. Arnold Paulino, a radiation oncologist affiliated with Methodist Hospital in Houston and lead author of the study.
Paulino sought to address these criticisms with new research presented at the 2008 annual meeting of the American Society for Radiation Oncology (ASTRO). The newer study produced nearly identical results to the 2002 trial, confirming that most pediatric medulloblastoma patients can be treated with IMRT without the risk of severe hearing loss.
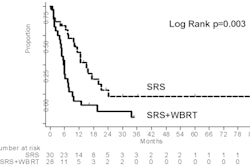
In the 2002 study, the incidence of ototoxicity was compared between children who received IMRT and those who received conventional radiation therapy. Only 13% of patients who received the IMRT boost developed grade 3 or 4 ototoxicity, compared with 64% who received the conventional boost.
In the newer study, Paulino's team included an additional 26 children receiving IMRT between 2001 and 2006, as well as the original cohort who represented the IMRT treatment arm.
Medulloblastoma, a tumor located in the cerebellum, accounts for 15% to 20% of all pediatric brain tumors. It affects approximately 500 children each year, ranging in age from infancy to age 18. After undergoing surgery to remove the tumor, patients receive a treatment combining craniospinal irradiation therapy followed by a posterior fossa and/or tumor bed boost. After that, most receive cisplatin-based chemotherapy, which is a well-documented cause of hearing loss.
Paulino and colleagues at Baylor College of Medicine and Texas Children's Hospital, both in Houston, wanted to prove or disprove the findings of the original clinical trial with a larger patient cohort and a longer follow-up period, as well as to determine if specific treatment actors that influence ototoxicity rates could be identified.
"Today, most pediatric oncologists use IMRT instead of conventional radiotherapy. The importance of our study is that its large sample size -- and, for some patients, nearly a decade of follow-up -- definitively validate the use of IMRT," Paulino said.
The cohort of patients receiving IMRT consisted of 30 boys and 11 girls, ranging in age from approximately three to 18 years (median age, nine years). Thirty-one of the patients were of standard risk, with no evidence of disease outside of the posterior fossa of the brain, and 10 were high risk, with either incomplete removal of the tumor and/or tumor spread elsewhere in the nervous system.
Standard-risk patients received 18-23.4 Gy of craniospinal irradiation, in which both ears are in the treatment field. This was followed by either a posterior fossa boost to 36 Gy and a tumor bed boost to 54-55.8 Gy, or a tumor bed boost alone at the same dose. High-risk patients received 36-39.6 Gy of craniospinal irradiation and the same boost treatments. For both types of patients, the cochlear dose was limited to approximately 40% of the dose prescribed for the posterior fossa and/or tumor bed boost. All patients received cisplatin-based chemotherapy, with a median dose of 300 mg/m2.
The researchers conducted and analyzed pure-tone audiograms at 11 to 92.4 months after treatment (median, 28.5 months). The Pediatric Oncology Group (POG) ototoxicity scale was used to grade the results of 82 ears.
|
The researchers determined that the degree of ototoxicity was not influenced by gender, age of the child at the time of treatment, the risk group, or the cisplatin dose. Patients who had no hearing loss did not receive a cochlear dose greater than 43 Gy.
"By using the IMRT cochlear-sparing approach, only 15.9% of the children developed POG grade 3 and 4 ototoxicity of cochlea treated," Paulino said. "These results are very similar to the 13% reported by Dr. Eugene Huang in the trial initiated in 1998 at Methodist Hospital."
By Cynthia E. Keen
AuntMinnie.com staff writer
January 19, 2009
Related Reading
Postop chemotherapy may replace radiation for pediatric medulloblastoma, March 11, 2005
White matter lesions following medulloblastoma therapy can mimic recurrence, December 1, 2004
Brain tumor irradiation tied to osteopenia in children, June 3, 2004
Copyright © 2009 AuntMinnie.com