No curative treatments exist for pancreatic cancer patients with locally advanced or unresectable disease. Various chemotherapy and chemoradiation treatments are used to enhance survival and improve the quality of a patient's remaining life. Should stereotactic body radiotherapy (SBRT) be one of these treatment options? That's open to debate.
Radiation oncologists at Stanford University in Stanford, CA, advocate its use, reporting local control and toxicity findings of a large clinical trial using SBRT (CyberKnife, Accuray, Sunnyvale, CA) to treat unresectable adenocarcinoma of the pancreas in a recent issue of Cancer (February 1, 2009, Vol. 115:3, pp. 665-672).
The study highlights the differing philosophies of two radiation oncologists who specialize in gastrointestinal cancers, one from the University of Texas M. D. Anderson Cancer Center in Houston and the other from Duke University Medical Center in Durham, NC. In an accompanying editorial, they suggest that more clinical trials be conducted before any opinion is reached.
The treatment
In 2002, Stanford's department of radiation oncology initiated a phase I dose escalation study to determine the feasibility of using SBRT, and to assess its toxicity on patients with locally advanced pancreatic cancer. This clinical trial and subsequent ones established the delivery of a single 25-Gy fraction of SBRT combined with systemic therapy as an institutional standard of care at Stanford.
SBRT has several advantages over conventional fractionated radiation therapy, including more intensified treatment to the primary tumor, increased patient convenience, and minimal interference with the delivery of maximal systemic chemotherapy, according to the researchers.
A total of 77 patients received SBRT treatment during a five-year period starting in October 2002. The majority (73%) of the patients had locally unresectable pancreatic adenocarcinoma. Nineteen percent had metastatic disease, 5% had medically inoperable tumors, and 3% had marginally resectable tumors.
Twelve percent of the patients had received prior radiation therapy, and 19% had completed chemotherapy. Seventy-seven percent were receiving chemotherapy at the time they were scheduled for SBRT treatment, and their chemotherapy treatment was halted for a 28-day period starting 14 days before the SBRT treatment.
Between 2002 and the beginning of 2004, a biphasic CT scan was used for radiation treatment planning; subsequently, 4D CT scans and PET scans were also utilized. The researchers defined the planning target volume for SBRT as the gross tumor volume plus 2 mm or 3 mm.
All patients received a single fraction of 25 Gy prescribed to the isodose line, completely covering 95% of the planning target volume. After treatment, patients received pancreatic-protocol CT scans and PET/CT scans at four to12 weeks after SBRT, and two to four months thereafter.
The results
As a result of SBRT, the tumor of one patient became resectable. The patient underwent surgery and remained alive and disease free as of October 2007, the end of the five-year clinical trial, some 12 months following surgery. However, lead author Dr. Daniel Chang, an assistant professor of radiation oncology at Stanford, and colleagues caution that SBRT is not an effective treatment for converting locally advanced disease to resectable disease.
The researchers defined both local and disease progression from the date of treatment to the date the first progression was documented. The range of patient follow-up for the study was three to 31 months, with an overall median of six months.
 |
||
| Summary of disease progression of the 77 patients | ||
 |
||
| 65 patients (84%) | Distant metastasis was first site of failure, of which 9 patients had metastatic disease at time of SBRT | |
 |
||
| 10 patients (13%) | Local progression as component of initial failure | |
 |
||
| 9 patients (12%) | Local progression in the regional lymph nodes | |
 |
||
| 4 patients (5%) | Isolated local failures | |
 |
||
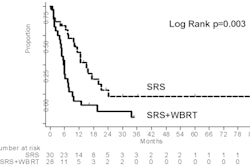
The rate of freedom from local progression for the entire group was 91% at six months and 84% at 12 months. By comparison, progression-free survival was 26% at six months and 9% at 12 months. Median survival durations were calculated from both time of diagnosis and time of SBRT treatment:
Four patients experienced acute toxicity within three months of treatment, two with a grade 2 small bowel ulcer, one with a grade 3 gastric ulcer, and one with grade 2 pain. Ten patients had late toxicity after three months, three with grade 2 small bowel ulcers, three with grade 3 gastric ulcers, one with grade 3 duodenal stricture, two with grade 3 biliary strictures, and one with grade 4 small bowel perforation.
One of the findings from the trial is that toxicity did not appear to hasten death of the patients. In fact, the median overall survival of patients from the time of SBRT treatment was 11.7 months. The researchers attribute this to the fact that the patients who lived longer were at higher risk of developing treatment morbidity.
From a patient perspective, one of the most important benefits of SBRT was significant reduction in pain, with the majority of patients experiencing improvement in pain management. The researchers hypothesize that more intensive local therapy should result in improved and more durable pain relief. Future clinical trials will include a longitudinal study of pain from pretreatment through follow-up.
Chang told AuntMinnie.com that for follow-up studies he and his colleagues want to study the kinetics of pain response, including times when pain diminishes/increases, how rapidly the changes occur, when pain disappears/reappears, and the duration for each type of pain level.
Future studies are also planned using fractionated SBRT with smaller doses per fraction in an attempt to reduce the risk of complications while maintaining excellent control. Chang and colleagues believe that their clinical trial proves that SBRT with 25 Gy delivered in a single fraction provides excellent local control, albeit with a risk of complications.
The rebuttal
Not as convinced of SBRT's efficacy are Dr. Christopher Crane, an associate professor of radiation oncology and section chief of gastrointestinal services at the University of Texas M. D. Anderson Cancer Center, and Dr. Christopher Willett, a specialist in gastrointestinal cancer and chairman of the department of radiation oncology at Duke University Medical Center.
In an accompanying editorial in Cancer, they stated that "SBRT is no more or perhaps even less efficacious than either chemotherapy alone or fractionated chemoradiation in the treatment of patients with locally advanced pancreatic cancer" based on the results of the Stanford study.
While noting that use of CyberKnife for patients who have primary or metastatic tumors of the lung or liver is attractive because these tumors move with aspiration, they cautioned that if the duodenum, small bowel, or stomach is inseparable from a pancreatic tumor, the duodenum cannot be avoided completely even if real-time motion tracking may minimize the volume of tissues that are treated. They expressed concern about pancreatic cancer patients' ability to tolerate treatment-related toxicity.
Crane and Willett do not believe that freedom from local progression can be used to assess the efficacy of local therapy. They argue that the time window to assess local progression was too short in the study, and because the median survival was also less than one year, the local control rates are of uncertain significance. Because pancreatic cancers are infiltrative with poorly defined borders, the difficulty of defining and quantifying pancreatic tumor size limits an accurate assessment of response and control, Crane and Willett stated.
Comparing the overall survival statistics of the Stanford patients with those of conventional treatments, Crane and Willett noted that tertiary centers evaluating various chemotherapy and chemoradiation strategies achieved medium survival durations between 14.4 and 19.1 months, and that the benchmark in locally advanced pancreatic cancer is approximately 15 to 19 months for single institution trials. The Stanford study did not achieve this.
SBRT as a therapy for advanced pancreatic cancers should be limited to institutional review board-approved clinical trials until better results are achieved, Crane and Willett concluded.
By Cynthia E. Keen
AuntMinnie.com staff writer
March 16, 2009
Related Reading
DNA variations may predict outcome in pancreas cancer, January 15, 2009
Perfusion CT predicts treatment response for pancreatic cancer, January 2, 2009
Extra therapy a plus after pancreas cancer surgery, January 22, 2007
Study shows CyberKnife capabilities with pancreatic cancer, May 26, 2004
Copyright © 2009 AuntMinnie.com
|