Active surveillance or chemotherapy work well for most men diagnosed with seminomatous testicular cancer, according to an analysis published in the Journal of Clinical Oncology of five-year outcomes of a community-based treatment protocol used throughout Norway and Sweden.
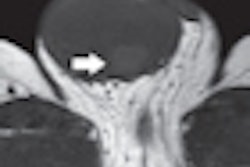
Concerns about radiation-induced secondary cancers led researchers to abandon radiation therapy for almost all patients, and to use MRI instead of CT as the standard mode of abdominal imaging for follow-up procedures (J Clin Oncol, January 4, 2011).
These were the major changes made in the Swedish and Norwegian Testicular Cancer Project (SWENOTECA) V, the fifth version of a protocol developed in 1981 to provide multidisciplinary, comprehensive management programs for the staging, treatment, and follow-up of testicular germ cell cancer.
The SWENOTECA-V protocol was used from January 2000 through December 2006, with 1,384 men receiving its recommended treatments. Lead author Torgrim Tandstad, MD, of the department of oncology of St. Olavs University Hospital in Trondheim, Norway, and co-authors reported that disease-free survival five years after treatment was 99.6%.
The majority of patients (86%) were diagnosed with clinical stage I seminomatous testicular cancer. Between 2000 and 2003, they were offered the option of active surveillance or radiation therapy to start within six weeks of orchiectomy, the surgical removal of one or both testicles.
In 2004, the additional option of chemotherapy, predominantly a single course of adjuvant carboplatin, was added. Forty-three percent of these patients chose surveillance only, 40% chose radiation therapy, and the remainder chose the chemotherapy option.
The majority of the 35 patients diagnosed with clinical stage IIA received radiation therapy consisting of 15 fractions of 1.8 Gy, for a total dose of 27 Gy, but six patients received chemotherapy instead. Patients with higher stages of disease received various chemotherapy treatments.
Follow-up protocols were determined by disease stage and therapy. The patients who elected surveillance had an average of 20 CT, MRI, or abdominal ultrasound exams over a 10-year period.
Among stage I patients, 65 (14.3%) of 512 relapsed following active surveillance, seven (3.9%) of 188 relapsed after carboplatin, and four (0.8%) of 481 relapsed after radiation therapy. The median time to relapse was 1.4 years for patients on surveillance, 1.8 years for those receiving carboplatin, and 1.1 years for those receiving radiation therapy.
Out of 102 patients with stage IIA/B disease, three patients relapsed, all of whom had received radiation therapy. The median time to relapse was 2.1 years. There were no relapses among the 73 patients who only received chemotherapy. The authors expressed concern about this outcome, although they pointed out that radiation therapy is no longer offered due to the risk of developing secondary cancers from radiation dose exposure.
The authors reported that they were unable to identify the prognostic factors for relapse in their analysis of tumor size, vascular invasion, age at orchiectomy, or human chorionic gonadotropin (hCG) level at orchiectomy. Because of this, they recommend that a prospective validation of proposed risk factors for relapse in stage I seminoma be initiated.
By Cynthia E. Keen
AuntMinnie.com staff writer
February 7, 2011