The fast pace of innovation and technological development in radiation oncology today can make it challenging to maintain an effective quality assurance program. So it's apropos that Practical Radiation Oncology tackles this subject in its inaugural issue.
Two lead articles in this new peer-review journal from the American Society for Radiation Oncology (ASTRO) describe how increasingly complex treatments and delivery systems can add to a practice's workload and workflow, subsequently undermining patient safety initiatives. The articles offer recommendations to deal with the challenges of increasingly life-saving and potentially lethal ever-evolving technologies (Practical Radiation Oncology, January-March 2011, Vol. 1:1, pp. 2-14, 16-21).
Changes need to be made by equipment and software developers. Radiation oncology departments need to adopt a safety culture that encourages questioning of decisions, rejects compromise for the sake of expediency, and adequately staffs positions commensurate with patient treatment workload to prevent overwork, distraction, and fatigue. Every single healthcare provider associated with radiation oncology needs to be proactive.
Today's fragmented reporting of errors, near misses, software and equipment glitches, and interconnectivity issues is ineffective. Radiation oncology professionals, vendors, and government regulatory agencies need to adopt an aviation-industry mindset.
It's time to adopt a systematic approach to identify root causes of errors that can lead to real patient harm, according to Lawrence Marks, MD, professor and chairman of the department of radiation oncology at the University of North Carolina at Chapel Hill. Common terminology needs to be developed and categories of errors need to be defined. It's time to eliminate ambiguities and abolish tolerance of underreporting, he believes.
Marks and his colleagues stress the need for central database repositories, where pooled data make it easier for radiation oncologists to identify problems that require immediate attention and take corrective action.
Defining new policies and procedures is no longer adequate to keep pace with change, according to the authors. Instead, the potential for risk needs to be minimized through tangible factors such as automation, standardization of products and processes, and use of checklists and redundancy. Root-cause analysis is needed to determine the origin of a mistake and how it can pass through the safety barriers that are in place.
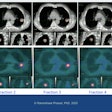
The adoption of advanced technologies, particularly image-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), has created information overload in departments that are also experiencing an increased volume of patients. Individual tasks are more interdependent and have more handoffs and opportunity for incomplete information transfer. The planning processes for IMRT, IGRT, and other 3D treatment technologies are more complex.
With IMRT, more data parameters need to be accurately calculated and transferred. This increases opportunities for mistakes to be made and information not communicated, the authors noted.
Other areas of vulnerability include the difficulty of detecting image segmentation errors and the reduced utility of some traditional quality assurance tools. Delivery of higher radiation doses to smaller targets and shorter, faster fractionation schedules can intensify the dosimetric and clinical effects of a single treatment deviation.
Meanwhile, heavy patient workloads may not allow treatment modality downtime, and may require rushed recalculation of treatment plans for use with different equipment. Even the use of electronic medical records (EMRs) may inadvertently generate erroneous documentation that could have been identified through the review of multiple-item, paper-based patient files.
Marks and colleagues also noted that use of more complex, automated treatments can instill a perception of infallibility and the assumption that systems will identify errors. Adopting good manufacturing practices (GMPs) can enhance safety practices.
The authors recommended that staffing levels need to reflect workloads, particularly for dosimetrists and physicists where demands have markedly increased. Clinical workflow should be analyzed through process maps, made as efficient as possible, and standardized. User-configurable checklists and time-outs need to be incorporated.
Communication among all department members is vital. Marks' department conducts a daily morning meeting that he likens to a sports team's "huddle." This meeting reviews treatment plans for new patients and covers the day's activities, providing a venue for constructive peer review and efficient pretreatment planning changes. It also serves as a forum to discuss the challenges of the workday and as a social event to promote open dialogue among all department members.
"Defining better policies is not enough," the authors wrote. "Ongoing changes in our clinical practice mandate continued vigilance."
AAPM/ASTRO safety meeting
But even more changes are needed.
Last summer, ASTRO and the American Association of Physicists in Medicine (AAPM) jointly sponsored a meeting to identify causes of mistakes and equipment failures in radiation oncology, and to develop approaches to rectify them. Convened as a response to a series of articles published in the New York Times exposing radiation oncology safety issues, the meeting attracted more than 400 medical physicists and dosimetrists, department administrators, radiation oncologists and therapists, representatives from regulatory agencies and professional organizations, and senior executives of the radiation oncology equipment industry.
In a separate article in Practical Radiation Oncology, William Hendee, PhD, professor of radiology, radiation oncology, biophysics, and community and public health at the Medical College of Wisconsin, and Michael Herman, PhD, professor of radiologic physics at the Mayo Clinic in Rochester, MN, reported on the recommendations that were made:
- Equipment that controls treatment devices should be simplified, standardized, and designed according to principles of human-factors engineering. Workstations should be clutter-free; present information in a logical, tiered fashion; and incorporate early warning systems that are more comprehensive and fail-safe and cannot be ignored.
- Early warning systems should include an automated treatment system and process checks that compare performance with established performance metrics. Solutions to make changes should be included, as appropriate, with the alerts.
- Radiation therapists must be knowledgeable about the correctness of radiation delivery to the patient during treatment. They should have the ability to stop a treatment.
- The U.S. Food and Drug Administration (FDA) review process should be improved. Integrity of interactivity of approved devices must be tested.
- Vendors should rapidly address problems and concerns reported to them. User alerts and user groups should be established.
- Norms for staffing levels based on workload should be established. Radiation therapists should not be expected to handle billing forms while patients are being treated.
- Error and root-cause analysis should be used to identify sources of errors and near misses and to correct problems. The objective should be to prevent or reduce the risk of similar errors occurring. Centralized, anonymous, nonpunitive error reporting systems should be developed. Procedures need to be developed and implemented for various regulatory agencies to be notified and to work together.
- Checklists and standard operating procedures should be utilized. Any member of the treatment team should be able to call a "time-out" to resolve questions or concerns about treatment.
- Audits of accuracy, quality, and safety should be conducted. Patient safety should be added as a core competency for radiologists, radiation oncologists, and medical physicists certified by the American Board of Radiology. Champions of patient safety should exist within every radiation oncology department to promote and maintain an overall culture of safety.
By Cynthia E. Keen
AuntMinnie.com staff writer
February 16, 2011