Adding radiation therapy and chemotherapy to lumpectomy for patients with ductal carcinoma in situ (DCIS) is more effective in reducing cancer recurrence in the ipsilateral breast than lumpectomy alone, according to a study published online March 11 in the Journal of the National Cancer Institute.
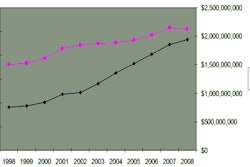
Cancer recurrence in the same breast is the most common "failure event" following lumpectomy for DCIS, according to a research team led by Dr. Irene Wapnir of Stanford University. At the same time, the prevalence rate of DCIS has been growing rapidly, largely due to increased use of mammography, to the point where DCIS now makes up some 25% of all new breast cancers (JNCI, March 16, 2011, Vol. 103:6, pp. 478-488).
The group wanted to explore whether adding additional treatments to lumpectomy would reduce the ipsilateral recurrence rate as well as patient mortality from DCIS.
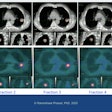
Wapnir's team looked at the long-term outcomes of patients with localized DCIS who took part in two large randomized trials, both carried out by the National Surgical Adjuvant Breast and Bowel Project (NSABP). The B-17 trial compared lumpectomy alone to lumpectomy plus radiation therapy in women with DCIS; its accrual period was October 1985 to December 1990. The B-24 trial compared lumpectomy plus radiation in combination with either tamoxifen or placebo, with an accrual period of May 1991 to April 1994.
The team analyzed data on outcomes in both trials after 15 years, including overall and breast cancer-specific survival, and survival after development of invasive breast cancer in the ipsilateral breast. Of 490 ipsilateral breast cancer recurrences, 263 (57%) were invasive, Wapnir and colleagues found.
The 15-year cumulative incidence of invasive ipsilateral breast tumor recurrence was as follows, according to the researchers:
- 19.4% for women who had lumpectomy only
- 8.9% for women who had lumpectomy following radiation therapy
- 10% for women who had lumpectomy following radiation therapy plus placebo
- 8.5% for women who had lumpectomy following radiation therapy plus tamoxifen
The findings point to the benefit of treating DCIS with more than just lumpectomy, according to the group.
"In spite of the fact that approximately 80% of the cancers in these trials were small clinically occult lesions, treatment by lumpectomy alone was associated with a relatively high incidence of invasive ipsilateral breast tumor recurrences, reaching 35% by 15 years," Wapnir and colleagues wrote.
The development of invasive ipsilateral breast cancer was associated with death rates that were statistically significantly higher than those in women who did not develop an invasive ipsilateral breast cancer, they wrote, although recurrence of DCIS was not associated with higher mortality.
For all patients in the trials, the group determined the following 15-year cumulative incidences of death from breast cancer:
- 3.1% for women who had lumpectomy only
- 4.7% for women who had lumpectomy following radiation therapy
- 2.7% for women who had lumpectomy following radiation therapy plus placebo
- 2.3% for women who had lumpectomy following radiation therapy plus tamoxifen
Some of these deaths could be attributed to new invasive contralateral breast cancers, according to Wapnir and colleagues.
DCIS rates aren't decreasing, they wrote -- and women who have the disease need treatment.
"The incidence of DCIS has risen over the past decade and may be continuing to do so," they wrote. "We believe that these long-term findings ... demonstrate that lumpectomy and adjuvant therapies are effective modalities for the treatment of DCIS."
Regarding limitations of the study, the authors noted that the results were based on trials conducted more than 20 years ago, when breast imaging technologies were inferior. The current study also did not evaluate women based on hormone receptor status.