Stereotactic body radiation therapy (SBRT) is a safe alternative to surgery for elderly patients diagnosed with stage I non-small cell lung cancer (NSCLC). This is true for patients considered to be medically inoperable and also those healthy enough to have surgery.
Does this recommendation represent a new standard of treatment? This question was posed -- and left unanswered -- during a discussion following the presentation of study results from VU University Medical Center in Amsterdam at the American Society for Radiation Oncology's (ASTRO) annual meeting.
Radiation oncologist Dr. Frank Lagerwaard presented data from a study of 177 patients treated at VU University's department of radiation oncology between 2003 and 2010, who had been retrospectively classified as being potentially operable. The patients had been selected from the hospital's database of 676 patients, each of whom a single primary lung cancer.
Lagerwaard and colleagues excluded patients who had received prior high-dose radiotherapy or undergone pneumonectomy. Patients were also excluded if they had undergone a chemotherapy and radiotherapy regime for a prior lung cancer, had major cardiovascular morbidity, had a concurrent malignancy, and/or had very severe chronic obstructive pulmonary disease (COPD).
The researchers ended up with a total of 177 potentially operable patients (101 men and 76 women; median age, 76 years), comprising 28% of their population who received SBRT. Patients were as old as 91, and 57% had considerable comorbidity.
"We didn't select the fittest of the fittest patients for this analysis," Lagerwaard said.
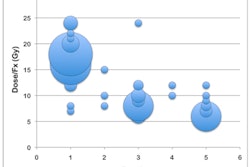
These patients received a 60-Gy radiation dose, delivered in three, five, or eight once-daily fractions administered over a one- to two-week time period. Fractionation was risk-adapted based on tumor location and size, with T1 tumors representing 60% of the group and T2 tumors 40%.
Toxicity was generally mild. There were no early side effects reported in 42% of the patients. One-fourth of the patients experienced fatigue as an early side effect. Fourteen percent developed a cough, 11% reported chest wall pain, and 10% had dyspnea. Some of the patients had more than one of these early toxicities, but only one patient had a grade 3 toxicity, which was chest pain.
Late toxicities consisted of rib fractures in 3%, chest wall pain in 3%, radiation-induced pneumonitis in 2%, and malignant pleural infusion in 1%. Grade 3 toxicity consisted of radiation pneumonitis in the chest wall, and a single patient suffered from grade 4 chest wall pain.
"If we look at the results of these potentially operable patients, with a median follow-up duration of almost three years, the median overall survival was 5.1 years," he said. "Three-year survival was 85%. Disappointingly, five-year survival was 51.3%."
The local control rate was 93% three years following SBRT, and regional and distant control were both 90% at three years, the researchers reported.
"What is important to note is that patients who underwent SBRT treatment had a lower risk of dying within the first 30 days following treatment than comparable patients who underwent surgery," Lagerwaard emphasized. "None of these patients died within the first 30 days, whereas the predicted 30-day mortality for a lobectomy derived using the Thoracoscore predictive model would have been 2.6% in this patient cohort."
The study findings support ongoing, randomized clinical trials that are comparing surgical and SBRT outcomes in potentially operable stage I NSCLC patients, he continued.
Noting that it is necessary to offer treatment recommendations based on outcomes that can be analyzed in SBRT databases of treatment centers throughout the world, Lagerwaard said that this study adds to evidence that SBRT offers an alternative to surgery for elderly patients with suspected or confirmed stage I NSCLC.
Lagerwaard also referenced an ASTRO poster presentation in which the research team tackled the issue of including patients suspected of having lung cancer who received SBRT. The high level of success of local control outcomes of patients treated with SBRT at the VU University Medical Center has been publicly criticized, Lagerwaard said.
The reason is because some of the patients whose outcomes were reported had suspected but unconfirmed lung cancer. Therefore, Lagerwaard and colleagues decided to determine if high outcomes were being achieved because patients with benign lesions were being treated.
They evaluated a cohort of 212 predominantly elderly patients diagnosed with pathologically confirmed stage I NSCLC before receiving treatment between 2003 and 2009. All of these patients had only single tumors, and 72% were considered to be medically inoperable; the remainder had refused surgery.
The patients had received a total dose of 60 Gy in a prescription of three, five, or eight fractions depending upon tumor size and location. This corresponded to biologically effective doses of 105 to 180 Gy. Toxicity was generally mild, with 3.4% of the patients experiencing at least grade 3 radiation pneumonitis chest wall toxicity within one year of treatment, and 7.8% within three years.
The median follow-up for this patient group was 31.5 months. Chest CT scans were performed every three months following treatment, and annually after 12 months.
One- and three-year survival rates were 83.1% and 55.8%, respectively. Eleven patients had a local cancer recurrence a median of 16 months following treatment.
"The local control rate of 89% proved to be in full agreement with our previously reported series," Lagerwaard said. "It is therefore unlikely that local control rates in these series had been biased by inclusion of benign lesions."