A new study has found that the adoption of brachytherapy-based accelerated partial-breast irradiation (APBI) has varied widely across the U.S., raising questions about whether the treatment is being used appropriately in breast cancer patients.
The study was published online ahead of print in the January 4 issue of the Journal of the National Cancer Institute. It comes just a week after a controversial study was presented at the San Antonio Breast Cancer Symposium, showing that patients who received APBI had higher complication and mastectomy rates than those who received whole-breast radiation treatment.
In the current study, researchers from Brigham and Women's Hospital examined a population of 138,815 women drawn from the Surveillance, Epidemiology, and End Results (SEER) database who were treated for breast cancer between 2000 and 2007.
The SEER data, which incorporate 17 tumor registries representing about one-fourth of the U.S. population, were linked to 2003 population-related data from the U.S. Department of Agriculture and to county-level sociodemographic information from the U.S. Census conducted in 2000 (JNCI, January 4, 2012, Vol. 104:1, pp. 29-41).
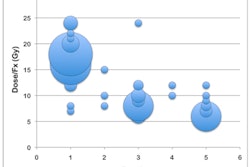
Radiation oncologist and lead author Dr. Jona Hattangadi and colleagues determined that 2.6% of patients in the SEER database received the APBI treatment. In 2007, 6.6% of the patients had APBI, compared with 0.4% in 2000, two years before the first commercial APBI catheter was cleared for use by the U.S. Food and Drug Administration.
The steepest increase in use was among patients categorized as suitable by 2009 American Society for Radiation Oncology (ASTRO) guidelines: from 0.7% in 2000 to 11% in 2007.
Utilization rates differed greatly among the 17 geographic regions for all categories of patients. The highest rates of utilization were in Atlanta (7%) and rural areas of Georgia (4.9%), and the lowest rates were in San Francisco (1.3%), San Jose (1.1%), and greater California (2.7%). The reason for this phenomenon is unclear, the authors wrote. However, they expressed concern "that APBI use is growing among patients who may not be suitable candidates for this radiation technique."
APBI utilization was greater among Caucasian women, with patients of other races half as likely to have received the treatment. The pattern of racial and ethnic variation in treatment may have reflected access to newer cancer treatment centers, which tended to offer APBI before other sites, the authors suggested. The phenomenon could also reflect different personal preferences by these groups.
Other findings included the following:
- Women older than 60 are twice as likely to receive APBI compared to women younger than 50 (3.4% of total versus 1.3%).
- Women living in cities who were categorized as "cautionary" for the treatment by ASTRO guidelines were more likely to have APBI than "cautionary" women living in rural areas.
- Women who underwent axillary dissections were less likely to receive APBI regardless of classification status.
- Almost twice as many women with invasive ductal carcinoma received APBI than patients with invasive lobular carcinoma, and larger tumor size was also a deterrent.
The findings are cause for concern, according to the authors.
"The wide geographic disparity in the use of APBI suggests that unwarranted variation -- practice variation not explained by illness, patient preference, or evidence-based medicine -- may be present, which can have a profound impact on healthcare costs and patient outcomes," they warned.
In an accompanying editorial, Dr. Simona Shaitelman, a radiation oncologist at MD Anderson Cancer Center, expressed concern about the fact that within this patient cohort, whose treatment preceded the ASTRO guidelines by two years, the majority of patients who underwent APBI were categorized as "unsuitable" (36%) or "cautionary" (30%).
This and two earlier published studies "raise an alarm that the care delivered to patients with early-stage breast cancer has evolved prematurely in relation to the results of large randomized trials examining the equivalency of APBI to [whole-breast irradiation]," she wrote.