Which end point of a clinical trial comparing cancer treatments is more important: disease-free or long-term survival? This question and others were raised in an article and editorial published in the New England Journal of Medicine on the long-term outcomes of Hodgkin's lymphoma patients.
Early-stage Hodgkin's lymphoma patients treated with multidrug chemotherapy alone were more likely to be alive 12 years later than patients who received treatment that included radiation therapy, reported principal investigator Dr. Ralph Meyer, of the National Cancer Institute of Canada (NCIC) Clinical Trials Group, and colleagues.
Findings from the phase III trial were published online December 11 in NEJM, and they were also presented at the American Society of Hematology's annual meeting, which was held December 10-13 in San Diego.
Meyer and colleagues reported the long-term findings of the Hodgkin's Disease.6 (HD.6) trial 17 years after it was initiated. The randomized trial compared outcomes of 405 patients with nonbulky stage IA or IIA Hodgkin's lymphoma who were treated with chemotherapy alone, subtotal nodal radiation therapy alone, or a combination of both treatments. The median age of the subjects was approximately 36 years when the study began.
The primary end point of the trial was survival: At 12 years, the rate of overall survival was 94% for the chemotherapy-only group, compared with 87% for those who received radiation therapy. Twelve patients in the chemotherapy-only group died, compared with 24 of the patients who receieved radiation therapy.
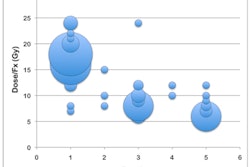
Cause of death in Hodgkin’s Disease.6 trial
|
The radiotherapy patients had a lower rate of disease recurrence, at 87%, compared with 92% for the chemotherapy-only group. The authors stressed that freedom from disease progression was not "a reliable surrogate marker for death, a far more important outcome," and they advocated that future trials involving Hodgkin's lymphoma patients should record cause of death to determine the percentage that could be treatment-related.
Today, the current treatment standard for patients with low-risk stage IA or IIA Hodgkin's disease, with lymph node masses smaller than 10 cm, is a combination of two cycles of chemotherapy with 20 Gy of involved-field radiation therapy. The radiation doses are a fraction of those used in the clinical trial and are limited to areas of the body affected by lymphoma.
This less-extensive radiation therapy and chemotherapy regime has resulted in the lowest rates of early relapse. In fact, enrollment in the HD.6 trial was closed prematurely, in April 2002, after results from the combination treatment were published. The date of final analysis also changed -- from December 31, 2015, to December 31, 2010 -- because the authors did not feel that the trial would reach its "goal" of 56 deaths by 2015.
The importance of this study is that it showed that chemotherapy alone prevented disease progression in all but 13% of the patients, Meyer said. Treatment with chemotherapy alone improves overall survival because it results in fewer late effects than radiotherapy, he noted.
Meyer acknowledged that current treatments have reduced late-toxicity risks, but he pointed out that clinicians do not yet know the magnitude by which they are reduced. Meyer and colleagues also suggested that the multidrug chemotherapy could be "more confidently" considered as a therapeutic option for this population.
"Although radiation therapy remains a useful tool for the treatment of some patients with Hodgkin's lymphoma, the challenge is to define the subgroup of patients for whom the benefits outweigh the increased risk of late complications," wrote Dr. David Straus, a hematologist on the lymphoma service at Memorial Sloan-Kettering Cancer Center, in an accompanying editorial.
Straus also agreed with the authors that long-term survival, rather than disease-free survival, was the most important outcome of treatment.
"With the availability of effective salvage treatment for relapses on the one hand, and the accumulation of late fatal treatment-related deaths on the other, long-term outcomes are probably more important than is the low early relapse rate," he wrote.