The combined treatment of chemotherapy and radiation therapy (RT) is more effective than radiation therapy alone for patients with muscle-invasive bladder cancer who don't have a cystectomy, according to a study to be published in the April 19 issue of the New England Journal of Medicine.
The results of the study offer some hope to frail, elderly patients of being able to maintain bladder preservation during the remainder of their lifetimes. The majority of patients who develop muscle-invasive bladder cancer tend to be in their 70s and older, and they face a sobering prognosis of a 44% chance of dying within five years from the disease.
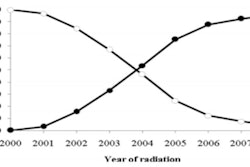
Among the 360 patients enrolled in a multicenter, randomized trial, those who had chemoradiotherapy had a 35% recurrence rate five years following treatment, compared with a 48% recurrence rate for patients who only received radiotherapy (NEJM, April 19, 2012, Vol. 366:16, pp. 1477-1488).
The clinical trial
The phase III trial was conducted at 45 cancer treatment centers in the U.K. to compare rates of survival-free locoregional disease, overall survival, and types and levels of toxicities for each treatment. An enrollment of 460 patients was originally planned.
Two-year outcomes of the clinical trial participants were originally presented at the 2010 American Society for Radiation Oncology (ASTRO) annual meeting by chief investigator Dr. Nicholas James, professor of clinical oncology at the University of Birmingham and consultant in clinical oncology at Queen Elizabeth Hospital. The current article presents updated findings.
Patients who enrolled in the trial between August 2001 and April 2008 were randomly assigned to undergo radiotherapy with synchronous chemotherapy (182 patients) or without it (178 patients) and either whole-bladder radiotherapy or modified-volume radiotherapy to the uninvolved bladder. The patients were predominantly male (30%) and elderly, with a median age of 72 years. The majority (82%) had a stage II primary tumor, while 17% had a stage III tumor.
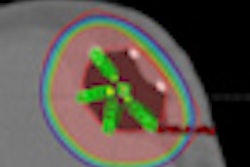
Radiotherapy was administered in one to two ways: as a four-week course of treatment of 20 fractions totaling 55 Gy; or over 6.5 weeks, with 32 fractions totaling 64 Gy. Patients assigned to the combined treatment arm of the study were administered chemotherapy during the first and third week of radiotherapy. Patients were followed for up to five years.
James and co-authors discovered that patients who had the combined treatment were much more likely to remain disease-free during the first two years following treatment than the radiotherapy group, at 67% versus 54%. Five years following treatment, this advantage increased to 13%.
Also at five years after treatment, more of the radiotherapy group had developed invasive bladder cancer than the chemoradiotherapy group (19.1% compared to 11.0%), as well as nonmuscle-invasive bladder cancer (16.9% compared to 14.3%). Twelve patients experienced pelvic node relapse in the radiotherapy group, compared with nine patients in the combined treatment group (6.7% versus 4.9%).
Death rates from bladder cancer were also higher in the radiotherapy group. Ninety-two patients, or 52% of the radiotherapy group, died of bladder cancer, compared with 74 patients, or 41%, of the chemoradiotherapy group.
James and colleagues had been concerned that the more intensive chemoradiotherapy treatment would cause more toxicities to their patients, they wrote. This was true during treatment, with 36.0% experiencing grade 3 or 4 toxicities, compared with 27.5% for the radiotherapy group. However, almost twice as many patients in the radiotherapy group (15.7%) experienced grade 3 and 4 late toxicities than in the chemoradiotherapy group (8.3%). In addition, if the category of sexual dysfunction is excluded, the late toxicity rates were nearly equal at 16.0% in the radiotherapy group and 16.9% in the chemoradiotherapy group.
Follow-up and additional observations
After enrollment in the clinical trial closed, new patients at Queen Elizabeth Hospital who did not undergo surgery were prescribed radiotherapy only, which represented the standard of care at the time, James told AuntMinnie.com.
However, as soon as interim outcomes were available after the majority of patients had reached the two-year mark after treatment, the trial management group decided to use the chemoradiotherapy regimen, and this has been the standard treatment since that time.
James and colleagues hope that, based on the five-year outcomes, the study will encourage oncologists and radiation oncologists to reevaluate the roles of bladder preservation and surgery in the treatment of muscle-invasive bladder cancer for all patients. For frail, elderly patients, recovery from surgery may be a difficult process.
"There is a widespread belief among surgeons that cystectomy is the standard of care," James said. "In fact, in many countries, radiotherapy treatment is not even offered to patients considered unfit for surgery." Many surgeons believe that radiotherapy will result in a small, poorly functioning bladder, he said.
The trial may help negate this belief. The researchers measured change in bladder volume one and two years following treatment: It was less than 10 mL and conclusively showed that radiotherapy does not routinely result in a small, shrunken bladder.
"Toxicity data also showed that over 70% of patients reported no bladder symptoms at all," he said. "We think that the good toxicity, low risk of death, and good functional outcomes demonstrated in an elderly group should result in many more patients being offered chemoradiotherapy treatment instead of surgery. Whether this happens will remain to be seen, of course."