The debate over the effectiveness of breast cancer treatment with accelerated partial-breast irradiation (APBI) brachytherapy has resurfaced with the publication of a paper critical of the technology in the May 1 issue of the Journal of the American Medical Association.
First presented in December at the San Antonio Breast Cancer Symposium (SABCS) by researchers from MD Anderson Cancer Center, the paper states that women treated with APBI had higher mastectomy and complication rates compared to those treated with whole-breast irradiation, the standard of care.
The article has drawn fire from APBI advocates, however, who express concern at what they say are flaws in the study that have not been rectified since it was first presented. They believe the research may inappropriately frighten patients newly diagnosed with breast cancer who qualify to receive the treatment -- and who might benefit from it (JAMA, May 1, 2012, Vol. 307:17, pp. 1827-1837).
The study
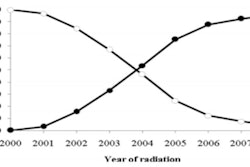
The population-based cohort study assessed Medicare claims of women older than 67 years who received either whole-breast radiation therapy or APBI breast brachytherapy between 2003 and 2007 and were followed through 2008.
While the initial SABCS presentation by Dr. Benjamin D. Smith, an assistant professor of radiation oncology at MD Anderson, referenced findings of 130,535 women treated between 2000 and 2007, the JAMA article focuses on five-year outcomes of 92,735 patients. Of these, 6,952 women, or 7.5%, received APBI treatments.
The authors determined that women who elected to have APBI had a nearly twofold increased risk (1.77%) of having a subsequent mastectomy. Smith and colleagues equated mastectomy with cancer recurrence. No data were presented as to whether mastectomies were based on patient choice.
It also was not possible from available data to determine if patients who had the APBI treatment were appropriate candidates for it. This was a criticism of the initial findings, and in the JAMA article, the authors address this possibility. Patients who had involved axillary lymph nodes were at particularly high risk of subsequent mastectomy if they had APBI instead of whole-breast irradiation, they noted.
"Evidence suggests that approximately 20% of patients treated with breast brachytherapy during the era spanned by our analysis fell into an 'unsuitable' treatment category as defined by the American Society of Therapeutic Radiology and Oncology Consensus Panel guidelines," the authors also wrote. APBI advocates believe the results might have been more favorable if the study was confined to patients who met clinical guidelines for the treatment.
The authors also acknowledged that the dataset used could not be adjusted for covariates such as cancer stage, histology, surgical margins, radiation dose, hormone receptor status, or endocrine therapy. All of these had been identified by critics as missing data that flawed the analysis.
With the exception of radiation pneumonitis, complication rates were higher for APBI-treated patients. Even though a smaller patient cohort over a shorter time period was used for the JAMA article compared to the SABCS presentation, complication rates were comparable to what had been reported in December 2011. Of note was the risk of infection within 12 months of treatment, at 27.6% for APBI-treated patients, compared with16.9% for patients receiving whole-breast irradiation.
The authors also suggested that the higher rate of mastectomy -- one performed for every 56 women who had APBI -- might be attributed to patients having multifocal or multicentric disease located outside the margin of breast tissue irradiated. However, the authors quote data from studies published in 1985 and 1996, without mentioning more recent studies that question or refute the earlier findings.
While they acknowledged the limitations of their observational study based on billing codes, Smith and colleagues wrote that performing a detailed analysis of clinical outcomes in a nonrandomized setting was warranted, in view of the lack of data and the controversy regarding widespread adoption of brachytherapy as the sole radiation treatment modality following breast conservation surgery.
The critics respond
Others continue to disagree. AuntMinnie.com interviewed a selection of breast surgeons and radiation oncologists who are proponents of offering APBI to patients who meet the guidelines for the procedure, as published by the American Society for Radiation Oncology in 2009.
APBI advocates have repeated their concerns, first raised in December, regarding the accuracy of the Medicare data. Also, the disparity in size between the two study cohorts, a more than 9-to-1 ratio, raises the prospect that any confounding factor could have a disproportionate impact on outcomes, according to Dr. Mary Katherine Hayes, associate professor of clinical radiation oncology at NewYork-Presbyterian/Weill Cornell Medical Center, and Dr. Martin Keisch, medical director of radiation oncology at University of Miami Hospital.
Both physicians were critical of the study's hypothesis that mastectomy was equated with cancer recurrence. Hayes pointed out that further investigation could have been undertaken to determine if patients who had a mastectomy had received additional treatment indicative of cancer recurrence. Keisch said that the decision to have a mastectomy could easily have been patient-related, such as a patient learning that she has the BRCA1 gene mutation and electing to have a prophylactic mastectomy.
"I applaud the effort here, but the methodology is flawed," Keisch said. "The paper looks worse than the abstract [presented at SABCS]."
The authors identified the percentages of complications between the two groups (which were at a level that none of the physicians interviewed said they see today). However, the authors failed to note that patients who had whole-breast irradiation were at greater risk for the most potentially serious complication, radiation pneumonitis, Keisch pointed out. While the chances of either group developing this were less than 1%, patients having whole-breast irradiation were four times more likely to develop the condition, he said.
"The authors use inflammatory language when talking about the percentage of patients who are harmed, especially when including patients who may not have been appropriate for treatment and were treated at a time when APBI breast brachytherapy treatment was at its infancy," said Dr. Douglas Arthur, professor and vice chairman of the department of radiation oncology at Virginia Commonwealth University (VCU) Massey Cancer Center.
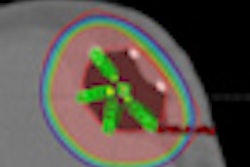
He pointed out that in its early years, especially between 2002 and 2006, only first-generation APBI applicators were available, and these were not as advanced in terms of radiation dose specificity. In addition, 3D conformal radiation treatment planning with CT was not commonly used.
"Things have changed dramatically with respect to the way that we prescribe the dose," Arthur said.
Infection control has also improved dramatically. Dr. Laurie Cuttino, a radiation oncologist at the Cancer Center at Henrico Doctors' Hospital and an associate professor at VCU Medical Center, noted that infection rates for both groups of patients are very low, and outcomes on all counts are comparable.
Cuttino recently published data demonstrating that 98% of patients treated with breast brachytherapy at VCU experienced good to excellent cosmetic outcomes, and significant late toxicity was uncommon. Only one of the many patients she's treated required a mastectomy for local recurrence after having APBI, she added.
Her experiences are echoed by oncologic breast surgeon Dr. Philip Israel, director of the Breast Center in Marietta, GA.
"The conclusions of the study are not consistent with what I've seen," Israel said. "Since 2002, we've performed over 1,000 APBI treatments. Outcomes are comparable with patients who undergo conventional radiation therapy."
"Let's put this study in perspective," Keisch said. "From a 10,000-ft level, what the authors are telling us is that whole-breast irradiation will increase local control by 2%. If 2% matters, all my patients should be asking for a mastectomy. Nobody is doing that."
"With the outcomes that are consistently being published in peer review publications about appropriately selected patients who've had APBI breast brachytherapy, I hope that new patients will realize this is an equally safe and effective procedure if it is offered to them," he said.
JAMA video comments by Smith
The JAMA article includes an accompanying interview with Smith explaining his findings.
Smith noted that "that there is a small but meaningful difference between patients treated with brachytherapy and whole-breast irradiation, although the outcomes for breast preservation for both groups were excellent. This led us to conclude that some of the trade-offs between whole-breast irradiation and brachytherapy may be a little bit more complex than previously appreciated or described in the medical literature."
After noting that his study’s findings are important for counseling patients to help them understand some of the trade-offs between the potential convenience of brachytherapy versus increased risks of complications and breast cancer recurrence, he turned to future research.
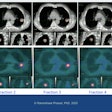
He pointed out the need to identify women who have the highest risk of breast cancer recurrence, regardless of the type of radiation therapy they receive. He also acknowledged the need to evaluate patients treated with brachytherapy in more recent years, noting that "techniques for brachytherapy continue to improve, and it is possible that with improvements in technique, we may see a difference."
Future studies comparing the outcomes of brachytherapy and whole-breast radiation-treated patients should include patients who only have a lumpectomy and do not have radiotherapy treatment, he said.
“It is important to note that in many of these patients, no radiation treatment at all is a reasonable option. ... Some of these patients may do just fine without any radiation, and then they would not be subject to the side effects of treatment,” he concluded.
The six-minute video can be accessed free of charge by clicking here.