FDG-PET/CT is useful for predicting the survival of breast cancer patients with hepatic metastases after treatment with selective internal radiation therapy, according to a study published in the March issue of the Journal of Nuclear Medicine.
Researchers from Ludwig-Maximilians-University of Munich concluded that FDG-PET was better able to determine which patients responded favorably to SIRT (radioembolization with microspheres containing the radioisotope yttrium-90) than CT or MRI. The lead author of the study is Dr. Alexander Haug from the university's department of nuclear medicine (JNM, March 2012, Vol. 53:3, pp. 371-377).
Previous research has found that approximately 20% of patients with localized breast cancer will develop metastases, despite advances in adjuvant treatment, Haug and colleagues noted. In recent years, radioembolization with yttrium-90 has become an effective palliative treatment for hepatic metastases of various tumors.
"In hepatic metastases of breast cancer, reported response rates to SIRT have ranged from 39% to 61%, with subsequent mean survival of two to 14 months," they wrote.
Compared with CT and MRI in other studies, FDG-PET has been shown to predict survival after therapy in patients with various types of tumors, according to the authors.
In this study, the researchers analyzed 58 women with a mean age of 58 years who were treated with yttrium-90 microspheres between March 2003 and October 2010. The mean interval between initial diagnosis and SIRT was 467 weeks ± 365 weeks.
Participants were older than 18 years of age and had confirmed cases of hepatic metastases from breast cancer. Subjects were excluded if they had liver failure or evidence of uncorrectable flow to the gastrointestinal tract, among other criteria.
Prior to therapy, all 58 patients underwent a whole-body FDG-PET/CT 3D scan (Gemini, Philips Healthcare, or Biograph 64, Siemens Healthcare) of three minutes per bed position. A short time later, patients underwent contrast-enhanced MRI of the liver.
Three months after radioembolization, the follow-up protocol included a physical examination, laboratory tests for liver function and other conditions, a contrast-enhanced MRI of the liver, and a second FDG-PET/CT scan.
To determine metabolic response using FDG-PET, the group measured the maximum standardized uptake value (SUVmax) of the hepatic metastases. The researchers summed the SUVmax values for up to five of the most notable hepatic metastases, and they compared the percentage change on the follow-up scan versus the baseline results.
A decrease greater than 30% of the baseline SUVmax would indicate that a patient responded favorably to therapy. However, a decrease less than 30%, any increase in SUVmax, or the appearance of new hepatic lesions would be considered an unfavorable or lack of response to therapy.
Among the 58 women in the study, 38 (65%) died during follow-up, leaving 20 women still alive after a mean follow-up of 27.5 weeks, ranging from 13 to 60 weeks. Response assessment with CT, MRI, and FDG-PET was available in 43 of 58 patients.
Overall median survival after SIRT was 47 weeks, and median survival after the initial diagnosis of breast cancer was 468 ± 341 weeks, the authors wrote. An SUVmax greater than 20 prior to therapy for the most intense hepatic metastasis per patient was associated with significantly shorter survival (median survival, 21 weeks) than an SUVmax of 20 or less (median survival, 52 weeks).
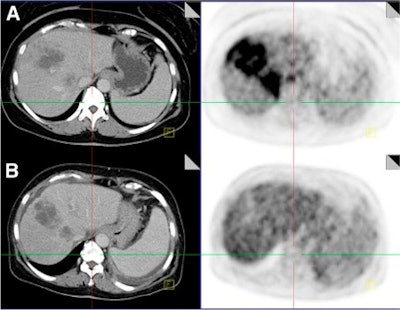 |
| CT images (left) and fused PET/CT images (right) were taken before therapy (A) and after therapy (B) and show large liver metastases. SUVmax decreased 273% after radioembolization, indicating therapy response, compared to tumor size measured by CT, which did not change significantly. Image courtesy of JNM. |
The study also showed that 22 participants (51%) responded favorably to therapy, while 21 (49%) did not fare well after treatment. Of those 21 women, seven (33%) experienced progressive disease based on the change in SUVmax. Therapy response based on SUVmax correlated significantly with survival after SIRT, with a median survival of 65 weeks for subjects who responded well to therapy, compared with 43 weeks for those who did not respond well after therapy.
Of the 43 patients whose CT and MRI findings were available, 11 (26%) had a partial response to therapy, 27 (63%) had stable disease, and five (11%) had progressive disease.
Haug and colleagues concluded that FDG-PET using SUVmax predicts survival of breast cancer patients with hepatic metastases treated with SIRT. "In multivariate analysis, the change in SUVmax was identified as the only independent predictor of survival," they wrote.
"Early identification of patients likely to experience poor outcome after SIRT permits the timely transition to alternative treatments," the authors added. "Despite the fact that these women [in the study] were heavily pretreated, further treatment options remain, which promise to improve their prognosis."