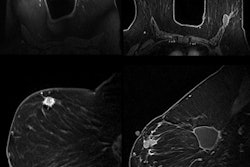
Women with early-stage breast cancer sometimes opt for mastectomy rather than less radical surgery out of concern about cancer recurrence. But recurrence risk was lower for women who chose lumpectomy followed by radiation therapy (RT) compared with those who received mastectomies, according to a study published online on Monday in Cancer.
Women in the study who underwent breast conservation surgery consisting of a lumpectomy followed by radiation therapy had better outcomes than those who had a mastectomy, the group from Duke University and the Cancer Prevention Institute of California concluded. This was particularly true for women 50 years of age and older who were hormone-receptor (HR) positive.
Another unexpected finding was that women who had mastectomies did not live as long as women who had breast conservation surgery. This proved consistent even after adjusting for age at diagnosis, year of diagnosis, tumor size and grade, and extent of lymph node involvement. The population-based study included more than 100,000 residents of California who were diagnosed with early-stage breast cancer between January 1, 1990, and December 31, 2004 (Cancer, January 28, 2013).
The researchers undertook the study to determine if outcomes in randomized, controlled trials for the two groups would also be observed in the general population. They used the California Cancer Registry to evaluate associations between surgery type, overall survival, and breast-cancer-specific survival. The researchers were particularly interested in evaluating the effects of age at diagnosis and hormone-receptor status.
The team led by Dr. E. Shelley Huang, chief of breast surgery at Duke Cancer Institute, identified 215,049 women ages 18 to 80 years. A total of 112,154 met the eligibility requirements for the study, which included being followed for at least five years. Forty-five percent (50,383 women) had undergone a mastectomy without any radiotherapy; the remainder, 61,771, had a lumpectomy followed by radiotherapy. The median follow-up time period was nine years.
Patient characteristics
The age of the patient did not have any effect on the type of treatment. The researchers categorized the women into five age groups, each of which had a similar percentage opting for either treatment. Division by race also produced similar percentages for each treatment group.
Women who received treatment in 1990, 1991, or 1992 were twice as likely to have a mastectomy. Starting in 1996, a higher percentage of women opted for breast conservation surgery, and this trend continued through the study period.
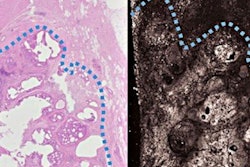
As might be expected, tumor stage and size affected treatment choice, with more women opting for breast conservation surgery if they were stage I, and almost twice as many women opting for mastectomy (9,723 patients) than breast conservation surgery (5,072) if they were stage IIB. Patients with larger tumors tended to have a mastectomy, as well as patients diagnosed with lobular cancers.
Outcomes
Long-term breast-cancer-specific survival for patients who had a lumpectomy and radiation therapy was either equivalent or superior to survival of mastectomy patients in all age groups and hormone-receptor types. Women at least 50 years of age with HR-positive tumors in the breast conservation cohort had 13% lower breast cancer mortality and 19% lower overall mortality than women who had mastectomies.
A total of 31,416 women died during the study period. Nearly 40% of deaths were attributed to breast cancer as the underlying cause. Among all patient groups, overall survival was better for patients who did not have a mastectomy.
The authors acknowledged that concurrent comorbidities, for which data were not available, could have affected overall survival. To try to determine if patients had comorbidities at the time of treatment, they conducted an analysis of deaths that occurred within three years following either treatment. Comorbidities did not seem to have an impact.
"These findings support the notion that breast conservation therapy, when combined with radiation, confers at least equivalent and perhaps even superior survival to mastectomy as definitive breast cancer treatment," the authors wrote.