Peer review is one of the most effective means for ensuring that radiation therapy decisions are tailored to specific patients, especially with respect to potentially controversial protocols. A new report in Practical Radiation Oncology defines peer review and discusses how it can be used in routine clinical practice.
The report is one of a series of white papers addressing patient safety that is part of an ongoing safety campaign by the American Society for Radiation Oncology (ASTRO). In addition to ASTRO, the campaign has been endorsed by the American College of Radiology (ACR), the American Association of Physicists in Medicine (AAPM), the American Association of Medical Dosimetrists (AAMD), and the American Society of Radiologic Technologists (ASRT).
The report fills a void, as little specific guidance has been issued by any medical professional society on patient-specific peer review, nor has much been published in the literature, according to a group led by Dr. Lawrence Marks, professor and chairman of the department of radiation oncology at the University of North Carolina School of Medicine.
The report concentrates on ways that peer review can be used to help improve the safety and quality of professional decisions made by the entire radiation oncology team in guiding treatment of specific patients. This team should include radiation oncologists, medical physicists, dosimetrists, and radiation therapists (Prac Radiat Oncol, March 16, 2013).
Marks and colleagues have created 26 items in six categories that define the process of radiotherapy as a potential target for peer review. The categories start with the initial decision to include radiotherapy as part of a patient's treatment program and, if appropriate, what should be done. Simulation, imaging, and patient immobilization represent the second category, followed by anatomical model definition. There are two segments related to specific treatment planning, including optimization planning, and plan preparation. The final segment relates to daily treatment.
It's not practical to address each of the 26 items included in the six categories all at once, according to the authors. They recommend that the items be categorized; those with a high potential risk to the patient and a low probability of the error being detected should receive the highest priority.
Top peer-review priorities
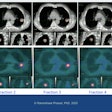
Of the highest priority is correct definition of the tumor target, including the need for multimodality imaging, fusion of the images, and the target definitions on the image.
"Every patient's tumor is different and visualization on different types of images can vary. Each image fusion is unique," the authors wrote. "Pretreatment peer review of how targets are defined ... is critical as mistargeting treatment can lead to poor clinical outcomes."
Clinical situations in which peer review is expected to be particularly useful include when stereotactic body radiation therapy (SBRT) is used, or when tumor margins are tight.
The first day of treatment delivery is also a high priority. Proper initial setup is critical to avoid systematic errors that may not be identified on ensuing days of treatment.
The authors recommend that peer review be performed on how radiation therapists set up the patient before the first treatment begins, and that it be performed again for all subsequent days of treatment. Portal or localization must also be done before the second treatment, with both medical physicists and radiation oncologists involved in quality assurance measures in the pretreatment stage.
Second-level priority items include the decision to include radiation as part of a patient's cancer treatment, as well as planning directive goals. These include dose/volume constraints and goals for irradiation levels of the target and of adjacent normal tissues. When these decisions are individualized and do not adhere specifically to best-practice recommendations, peer review is recommended.
Evaluating the treatment plan in terms of its ability to achieve desired dose/volume results is also categorized as a second-level priority. Normal tissue dose/volume guidance documents are generally available, but the compromises between normal tissue versus target doses are often patient-specific. The objective of peer review is to eliminate the need to make midtreatment changes.
Implementing a peer-review program
The authors bluntly state that implementing an effective peer-review program can be challenging. Support by executive-level management is mandatory because in addition to allocating the necessary resources and time, a positive rather than punitive culture needs to be established. The report identifies 13 common barriers or challenges to implementing an effective program, and it offers detailed recommendations and potential intervention techniques. As one example, it recommends that small treatment centers without a large clinical staff implement peer review to collaborate with other small, noncompeting centers.
The authors also emphasized the need for software designed to support and facilitate peer review of individual patient cases. They recommend that peer-review tools be integrated into routine workflow -- embedded, for example, within treatment planning/management systems. They also recommend that radiation oncology software planning programs have tools to streamline peer review of target doses and prescriptions and normal tissue exposures, as well as for facilitating review of segmented anatomy.
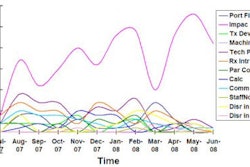
Intercenter connectivity is also very important, particularly for small centers that may need to establish peer review with a noncompetitive center. A current example of multicenter case discussion is Chartrounds, a program designed to facilitate discussion of patient-specific treatment plans by any vetted radiation oncology professional in the world. This model could just as easily focus on patient-specific peer review.
A copy of ASTRO's white paper can be accessed here.