New uses abound for 3D printing -- and now you can add radiation therapy to the list. A Canadian medical physicist has developed a 3D printing technique that converts data from CT scans of patients into wearable pads that help radiation beams conform to patient anatomy.
The 3D printed pads, called boluses, can be used for multiple indications, including external-beam radiation therapy in patients undergoing treatment after lumpectomy and photon treatment for women who have had a mastectomy. They can also be used for patients being treated for skin cancers and head and neck cancers.
"The bolus can be designed and printed with a specific shape, so we can conform the 3D dose distribution so that it matches the shape of the lumpectomy cavity," explained James Robar, PhD, chief of medical physics at the Nova Scotia Health Authority in Halifax, Nova Scotia, in an interview with AuntMinnie.com. Robar is also an associate professor of radiation oncology at Dalhousie University in Halifax.
Correcting for irregularities
In radiation therapy, a bolus is used during treatment to correct for anatomical irregularities and deliver the correct radiation dose to the target area. For example, during radiation after breast-conserving therapy, a bolus placed on the area to be irradiated can shift the depth of dose distribution.
But conventional boluses made from polymers are less than optimal if they don't conform exactly to a patient's anatomy.
"The chest wall can have a very irregular shape after mastectomy," Robar explained. "It's challenging to use the standard polymer bolus if it is not being placed on a smooth surface and there is irregularity. Air cavities between the bolus and the skin can cause an underdose to the surface of the patient."
But a 3D-printed bolus is based on the patient's own CT image data, so the printed bolus conforms well to the chest wall.
"There needs to be a good fit, so that we deliver a uniform and sufficient radiation dose to the chest wall that will eradicate cancer cells on the surface," Robar said.
For example, a 3D wearable bolus in electron radiation therapy for a woman who has undergone a lumpectomy allows for a sufficient and conformal dose of radiation to be administered to the lumpectomy cavity.
The tailored device can also be used for chest wall photon treatment, ensuring optimal radiation exposure for patients who have undergone mastectomy, he said.
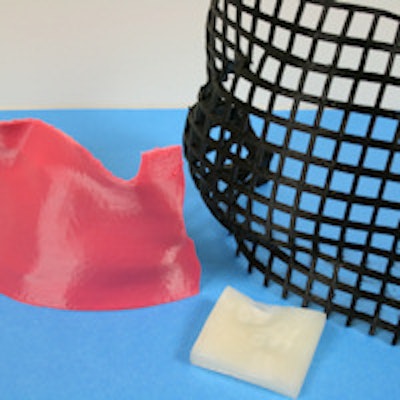
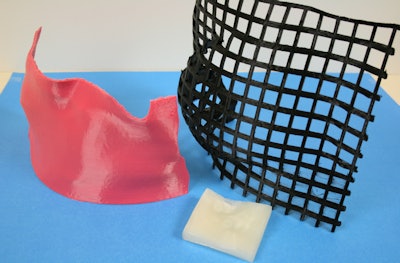 A customized chest-wall bolus (left) was 3D printed using a flexible, tissue-equivalent material that conforms to the patient's shape. A "smart bolus" (middle) was designed for electron beam therapy, where the surface shape of the bolus modulates the electron beam to achieve conformity of the radiation dose distribution to the tumor volume below. A low-density immobilization device (right) was designed to achieve reproducibility in patient positioning over the course of breast radiotherapy, while minimizing acute toxicity. Image courtesy of James Robar, PhD.
A customized chest-wall bolus (left) was 3D printed using a flexible, tissue-equivalent material that conforms to the patient's shape. A "smart bolus" (middle) was designed for electron beam therapy, where the surface shape of the bolus modulates the electron beam to achieve conformity of the radiation dose distribution to the tumor volume below. A low-density immobilization device (right) was designed to achieve reproducibility in patient positioning over the course of breast radiotherapy, while minimizing acute toxicity. Image courtesy of James Robar, PhD.The bolus design algorithm addresses target volumes with variable shapes, location, and distance to organs at risk. The material that has been used for the 3D printed bolus is polylactic acid (PLA), a solid printable material derived from starches, but Robar noted that PLA may not be optimal.
"PLA printed bolus is quite rigid, so that may be a potential drawback," he said. "There is a possibility that if a chest wall patient moves her arm, for example, before radiation treatment, that would create an air gap."
Consequently, the team in Halifax is now investigating printable and flexible materials that also simulate the radiological properties of tissue.
"We are able to perform conebeam imaging of patients to determine if there are any air cavities between the bolus and the skin," he noted.
Robar and colleagues plan to conduct a single-center study with 16 mastectomy patients to compare treatment using the conventional material versus the 3D printed bolus.
"We will take CT images to assess the spatial accuracy of the 3D printed bolus," he said. "We will also use in vivo optically stimulated luminescent dosimeters to measure the dose [of radiation] on the surface of the chest wall to compare to the status quo bolus with regard to dosimetric accuracy."
Another advantage of the 3D-printed bolus is that neither patients nor staff members need to be present during the process of bolus fabrication. Compared with manual bolus fabrication, with thermoplastics, for example, the customized bolus is designed using the researchers' own software and produced in an automated fashion.
Robar and colleagues hold a patent on the 3D-printed bolus technique and are working with Dalhousie University's Industry Liaison and Innovation office to license and commercialize the technology. To that end, they are reaching out to established firms in the radiation oncology space, seeking funding to advance the technology for wider use.
"The goal would be for a partner to move this through development, regulatory approval, and market launch," said Doris Grant, an associate director at the industry liaison office. "Our goal is to help get the technology to patients."
Robar and Grant will attend the American Society for Radiation Oncology (ASTRO) meeting being held October 18-21 in San Antonio, with an aim to meet face to face with prospective partners for the 3D-printed bolus technology.
While it's still early, Robar predicts that the technology will become more precise and rapid, and that more materials will be available to fabricate the bolus.