U.S. researchers say they have developed a new 3D imaging prototype for visualizing real-time radiation dose in patients undergoing radiation therapy. They published the results of their study on January 2 in Nature Biotechnology.
The prototype is based on ionizing radiation acoustic imaging (iRAI), a noninvasive imaging technology that reconstructs radiation doses using acoustic waves. These waves stem from the absorption of pulsed x-ray beams in soft tissue. In testing, the system provided real-time 3D visualization of the radiation dose delivered to a patient with liver metastases.
"In future applications, this technology can be used to personalize and adapt each radiation treatment to assure normal tissues are kept to a safe dose and that the tumor receives the dose intended," said co-author Dr. Kyle Cuneo, a radiation oncologist at the University of Michigan in Ann Arbor, in a news release from the university.
Successful radiation therapy in cancer patients is contingent on delivering sufficient radiation doses to tumors while sparing surrounding normal tissues. Maximizing tumor control while minimizing toxicity requires that the planned radiation dose is delivered accurately. However, current techniques to visualize dose are ultimately limited by normal tissue motion, the authors wrote.
The experimental prototype leverages the thermal energy of x-rays absorbed by tissue in the body. The heating causes the tissue to expand rapidly, and the expansion creates a sound wave. This acoustic wave is weak and usually undetectable by typical ultrasound technology.
The prototype iRAI system detects this wave with an array of ultrasonic transducers positioned on the patient's side. The signal is amplified and then transferred into an ultrasound device for image reconstruction.
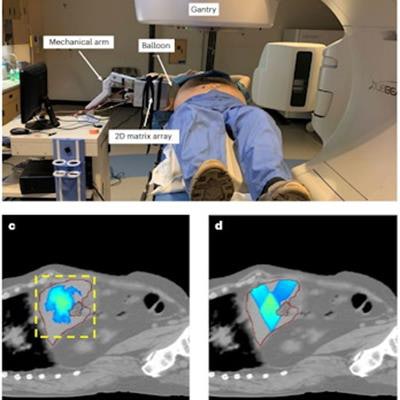
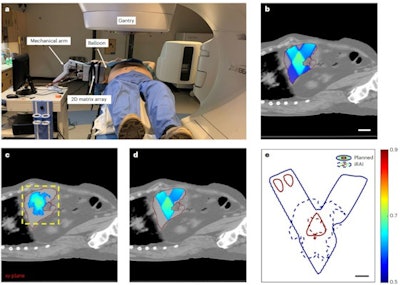 In vivo iRAI imaging versus the treatment plan on a patient. (a) A photograph of the iRAI imaging on a patient taken during RT. (b) The dose distribution of only the two static sagittal beams of the treatment plan with a liver mask fused onto the CT scan anatomy structure. Scale bar, 5 cm. (c) The iRAI measurement of dose with a liver mask fused onto the CT anatomy structure with the same position as in (b). The yellow dashed box indicates the field of view of the 2D matrix array. (d) Dose distribution (> 50%) of the treatment plan with a liver mask fused on the CT anatomy structure. (e) The 50 and 90% isodose lines in the iRAI measurement and the treatment plan. Scale bar, 2 cm. The red line (b-d) indicates the boundary of the liver. Images and caption courtesy of Nature Biotechnology through CC BY 4.0.
In vivo iRAI imaging versus the treatment plan on a patient. (a) A photograph of the iRAI imaging on a patient taken during RT. (b) The dose distribution of only the two static sagittal beams of the treatment plan with a liver mask fused onto the CT scan anatomy structure. Scale bar, 5 cm. (c) The iRAI measurement of dose with a liver mask fused onto the CT anatomy structure with the same position as in (b). The yellow dashed box indicates the field of view of the 2D matrix array. (d) Dose distribution (> 50%) of the treatment plan with a liver mask fused on the CT anatomy structure. (e) The 50 and 90% isodose lines in the iRAI measurement and the treatment plan. Scale bar, 2 cm. The red line (b-d) indicates the boundary of the liver. Images and caption courtesy of Nature Biotechnology through CC BY 4.0.In the study, the researchers first validated the feasibility of imaging temporal 3D dose accumulation in an anthropomorphic phantom. Next, they verified semiquantitative iRAI relative dose measurements in a rabbit model. Finally, they tested the system for visualizing radiation dose in a patient with liver metastases.
In both the rabbit model and the patient, the iRAI measurement clearly visualized a dose distribution similar to that of the treatment plan in vivo without interrupting the treatment delivery, they found.
Ultimately, with such images in hand, oncology clinicians could alter the level or trajectory of radiation during radiation therapy procedures to ensure safer and more effective treatments, according to the group.
"Although the treatment plans for both the rabbit model and the patient are relatively simpler than common treatment planning procedures, the results from this study demonstrated that the iRAI is a clinically feasible and practical technique," Cuneo and colleagues concluded.