MRI-guided focused ultrasound surgery (MRgFUS) is superior to external-beam radiation therapy (EBRT) for relieving pain in patients with bone metastases, according to Italian research published January 3 in Radiology.
A team led by Dr. Alessandro Napoli, PhD, from Sapienza University of Rome found that MRgFUS yielded higher response rates, lower pain scores, lower adverse event rates, and improved quality of life in patients compared with EBRT.
"The main advantages of MRI-guided focused ultrasound compared with EBRT are the absence of ionizing radiation and the ability to induce pain relief within a few days," Napoli and co-authors wrote.
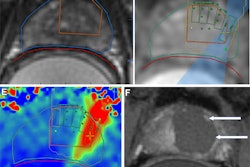
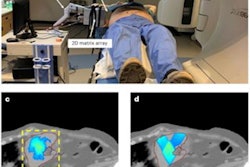
MRI-guided focused ultrasound surgery has been highlighted in recent years for its ability to treat several benign and malignant conditions with higher accuracy in tumor targeting.
However, the technique has had limited use for relieving suffering in patients with painful bone metastases. The researchers noted that this is because of a lack of data comparing this method with EBRT, the standard of care in this area. They also highlighted the surgical ultrasound method's ability to guide tumor treatment without damaging healthy surrounding tissues.
The Napoli team wanted to compare the two treatment methods in palliative care and treatment of bone metastases in a nonrandomized phase II study. They looked at retrospective data collected from 198 patients between 2017 and 2019. Out of these, 100 underwent MRI-guided focused ultrasound surgery and 98 underwent EBRT.
The team looked at overall response rates at one- and 12-months following treatment, as well as pain levels reported by patients, using a 0-to-10 numeric pain scale. Zero represents no pain, while 10 represents "the worst pain imaginable."
The researchers reported that MRgFUS resulted in significantly higher response rates and lower pain scores on follow-up.
| Performances in treating painful bone metastases | |||
| EBRT | MRI-guided focused ultrasound surgery | p-values | |
| Response rates at one-month follow-up | 67% | 91% | < 0.001 |
| Complete response rates | 16% | 43% | < 0.001 |
| Baseline pain scores | 6.6 | 7.0 | 0.16 |
| Pain scores at one-month follow-up | 5.1 | 3.2 | < 0.001 |
The researchers also looked at Quality of Life-Questionnaire Cancer-15 Palliative Care (QLQ-C15-PAL) scores. They found that scores for physical function, appetite, nausea and vomiting, dyspnea, and quality of life were significantly lower in the MRgFUS group.
Additionally, the overall adverse event rates were 15% after focused ultrasound and 24% after EBRT.
The study authors wrote that while randomized trials are needed to further investigate these results, they highlighted that they "provide the foundation" to construct a phase III trial with baseline estimates of response.
In an accompanying editorial, Dr. Alexis Kelekis, PhD, from the National and Kapodistrian University of Athens in Greece wrote that future studies in this area should try explaining these results based on different mechanisms of action for the two methods.
"Perhaps the future lies in combined therapies and hybrid techniques trying to bridge and exploit the advantages of each therapeutic approach," he wrote.
Kelekis also wrote about the ethical and logistical challenges of randomized trials for "vulnerable" patients in this population.
"We have placed randomized control trials on a high pedestal," he added. "However, statistical tools, such as propensity score matching, may become an alternative to randomization, providing a different approach of equally high-quality data."