When paired with other modalities, breast ultrasound can reduce the need for biopsy, but imaging lesions with sonography alone may not be reliable enough to completely bypass the procedure. By the same token, optical tomography reveals vital information on tumor angiogenesis and hypoxia, but imaging resolution is limited by technical issues. The combination of the two modalities may be the ticket to differentiating benign and malignant breast masses.
"Information on lesion structure that is provided by other modalities can be used to assist optical imaging reconstruction and thereby reduce location uncertainty and improve the quantification accuracy of light," wrote Quing Zhu, Ph.D., and colleagues in Radiology (October 2005, Vol. 237:1, pp. 57-66).
Zhu and several co-authors are from the bioengineering program at the University of Connecticut in Storrs. Drs. Edward Cronin, Allen Currier, and Hugh Vine, radiologists at Hartford Hospital in Hartford, CT, also contributed to this research.
In addition to testing the feasibility of US-guided optical tomography, the authors compared this method to color Doppler ultrasound. From May 2003 to March 2004, 65 women (mean age of 51 years) with 81 lesions were enrolled in the study.
Sonography was performed with spatial image compounding and a 14-MHz linear transducer (15L8 Sequoia, Acuson/Siemens Medical Solutions, Malvern, PA). The handheld optical-US hybrid probe consisted of a commercially available transducer and near-infrared optical fibers. The transducer was located in the middle of the probe, while the optical light detectors were at the periphery. For each patient, ultrasound images and optical measurements were acquired simultaneously prior to biopsy.
According to the results, there were eight early-stage invasive carcinomas and 73 benign tumors including fibroadenoma, fibrocystic change, and complex cysts. The total hemoglobin concentration was more than twofold higher in the malignant lesions.
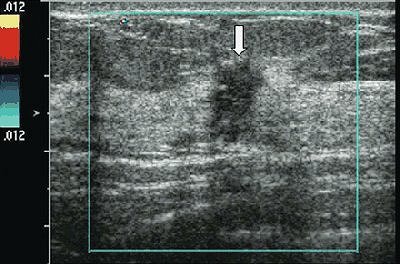 |
| US image and hemoglobin concentration maps of infiltrating lobular carcinoma (nuclear grade 2-3) located at 12 o'clock position in right breast of 37-year-old woman. Above, US image demonstrates lesion (arrow) measuring 1 cm in diameter. No blood vessels or blood flow were seen at color Doppler US. Below, total hemoglobin concentration map computed from absorption maps (not shown) obtained at 780 nm and 830 nm. Hemoglobin map reveals isolated high concentration mass in sections three (slice #3) and four (slice #4). Maximum hemoglobin concentration was 102.1 µmol/L, and average hemoglobin concentration was 68.7 µmol/L, as measured within FWHM region. Vertical scale presents total hemoglobin concentration in micromoles and ranges from 0 to 150 µmol/L. |
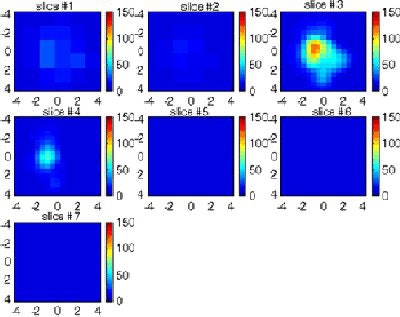 |
| Figure 5a,b. Zhu Q, Cronin EB, Currier AA, et al. "Benign versus malignant breast masses: optical differentiation with US-guided optical imaging reconstruction." Radiology 2005;237(1);57-66. |
The authors found that the sensitivity of US-guided optical tomography was 100%, the specificity was 96%, the positive predictive value (PPV) was 73%, and the negative predictive value (NPV) was 100%. In comparison, the sensitivity of color Doppler ultrasound was 63%, the specificity was 69%, the PPV was 19%, and the NPV was 94%.
"We believe that our technique ... has demonstrated great potential to noninvasively distinguish malignant from benign masses, and thereby potentially reduce the number of benign biopsies," the authors concluded, calling for larger prospective clinical trials.
Some of the issues that need to be addressed in future research are optical tomography's limitations in imaging lesions that are located close to dark nipple-areolar tissue and poor probe-to-tissue contact in small, dense breasts.
"Women who would benefit from (US-guided optical tomography) would be those with suspicious, smaller lesions visible on US," Zhu explained in an e-mail to AuntMinnie.com. "We have found that smaller dense breasts may cause optical imaging artifacts. However, large dense breasts and skin color do not seem to affect optical imaging results on cancer diagnosis."
Zhu's group will continue to work with US-guided optical tomography in an expanded patient population, she said. A second study by the group indicated that the technique was useful for monitoring postchemotherapeutic response of large cancers (Neoplasia, March 2005, Vol. 7:3, pp. 263-270).
In addition, the handheld probe can easily be operated by a trained ultrasonographer, Zhu said. While this experimental modality is not currently covered by Medicare, Zhu estimated that it will ultimately turn out to be more cost-effective than biopsy, although it will never replace biopsy altogether.
By Shalmali Pal
AuntMinnie.com staff writer
October 13, 2005
Related Reading
Avoiding false negatives on breast ultrasound, September 23, 2005
Compression US plus computer analysis classifies solid breast masses, September 7, 2005
Before breast screening, women want the lowdown on logistics, callbacks, June 27, 2005
Ultrasound helps find occult breast cancer postsurgery, May 4, 2005
Copyright © 2005 AuntMinnie.com