Echocardiography, already the most versatile cardiac imaging tool in the box, is poised to get a lot better in the years to come. Many promising applications -- in transducers, miniaturization, and visualization and quantification of cardiac function -- are already developed and operational. More are on the way.
The biggest change in the near future will likely be in broader access to advanced technologies that have already been invented -- delivering more of it to more clinicians, according to a presentation earlier this month at the Integrated Imaging in Clinical Cardiovascular Practice meeting in San Francisco. In his opening presentation, Dr. James Thomas, director of the three-day course sponsored by the American College of Cardiology (ACC) Foundation, ticked off a few advantages echocardiography can claim already.
"It has high temporal and spatial resolution. It's tomographic with a 3D option. You can do velocity and flow quantitation. It's noninvasive, nonionizing, nonmagnetizing, portable, miniaturizable, low-cost, and low-power," said Thomas, who is also the chief of cardiac imaging at the Cleveland Clinic Foundation in Ohio.
Add to that a host of new developments under way in 3D echocardiography, color Doppler quantification, left ventricular (LV) function assessment, contrast perfusion, and targeted imaging, he said.
"What will drive innovation in echo? You cannot change the laws of physics. The speed of sound will remain 1,540 m/sec in tissue, the maximum useful frequency in adults will be somewhere between 3-5 mHz pulse, and color Doppler will still alias," Thomas said. "But we can improve data extraction; we can build better transducers with less noise, ringing, etc. We can have quieter amplifiers, which are key to harmonic imaging, and we can ride the never-ending wave that is Moore's law."
But even Gordon Moore, who famously predicted in 1965 that computing power would double every 12 to 24 months, could be considered a pessimist if one were to look at the growth in ultrasound technology, Thomas said. The number of transistors per chip doubled every 26 months from about 4,000 in 1971 to 1 million today. Since 1999, the rate has been accelerating, Thomas said.
"What can we do with this magically increasing processing power? We can keep the features the same and keep the package small, or keep the same size package and make the features more powerful," he said.
In fact, developers have enthusiastically been doing both. A whole array of miniaturize echocardiography machines is offering increasing functionality in a small package -- like an echo system on a laptop. One such system has built all the beam-forming elements into the probe and connector, which hooks up to an off-the-shelf PC. In addition, wireless telemetry systems offer real-time ultrasound review, Thomas said.
"3D echo has really come a long way. It used to take months to extract real-time data. Now we've moved to 3D echo using 2D array (transducers) with crystals so small they rival the size of a human hair," he said.
These arrays can scan in any direction; 16:1 parallel processing can yield 64 scan lines in 64 scan planes in 25-40 msec. 3D echo exams can be performed in one to two minutes with high accuracy, and rudimentary color Doppler has been incorporated into the exams.
"Reconstructed echo is getting better as well," Thomas said. With respiratory and cardiac gating, echo planes are acquired every 3° to 5° by transesophageal echocardiography.
Thanks to more powerful processors and software, 3D echocardiography is delivering better and more realistic displays and navigation, and improved registration between successive studies. This enables tests, such as pre- and postexercise scans, to be readily compared, Thomas said. There is also cross-modality registration for some applications, automated segmentation and quantitation, and finally, better 3D image compression and 3D parametric imaging.
By now, multiple studies have demonstrated the accuracy of ultrasound measurements of the heart, including an early paper by Qin et al, who found the accuracy of LV volume measurements in 3D echo to be well-correlated with MRI (Journal of the American College of Cardiology, September 2000, Vol. 36:3, pp. 900-907). But the process is much faster now, with an ever-growing range of measurements, Thomas said.
| Apical 3D echocardiography of a cleft mitral valve, looking down onto the anterior leaflet from the left ventricular outflow tract. All images and videos courtesy of Dr. James Thomas. Having trouble viewing this clip? Click here to view full size clip or to change format. |
Manual measurements used to take hours. "In the bad old days, quantitation required a (medical) fellow with no life (outside the lab)," Thomas said. But these days 3D echo analysis is increasingly automated, increasingly rapid, and can be expected to continue its evolution. For example, "just the algorithms for detecting surfaces will be getting better and even more useful," he said.
Parametric displays of 3D echo data aren't just for analyzing heart structures, he said. They can assess things like cardiac synchrony, where an echocardiography time-to-peak velocity calculation showed good synchrony in the region of the lower left ventricle.
| 3D echo of a patient with a bicuspid AVR and posteriorly directed aortic regurgitation. Having trouble viewing this clip? Click here to view full size clip or to change format. |
"Color Doppler quantification is something we're doing in a rudimentary fashion," Thomas said. "For the most part, we just look at the colors and we describe things morphologically, but it's actually possible to use the velocities within those colors and not just the colors themselves."
Ten years have passed since researchers first quantified LV outflow by integrating color Doppler across the LV outflow tract in space and time with good accuracy, Thomas said. In the coming years, it's probably a safe bet that "stroke volumes will be readily available on all of our patients just by pushing a button," he said.
Imaging the proximal flow convergence region in the aorta looks for blood flow that accelerates in a retrograde fashion across the aortic valve. Useful for identifying the site of regurgitation and assessing its severity, these measurements have traditionally been performed with MRI. But they are increasingly being performed with ultrasound, which is adding its own functionality. The technique will only grow more accurate in the coming years, Thomas said, and echo will measure more and different flow velocities in the atrial region.
"These are very tiny (intraventricular) pressure gradients which represent diastolic suction of 2-3 mm mercury that pull blood into the ventricle and make the ventricle fill efficiently," he said. "They have been almost impossible to measure before echo. Now we can do it with color Doppler with good accuracy."
And it's not just for systole anymore. A group in Spain applied the method to diastolic measurements with good accuracy (Yotti R et al, Circulation [in press]).
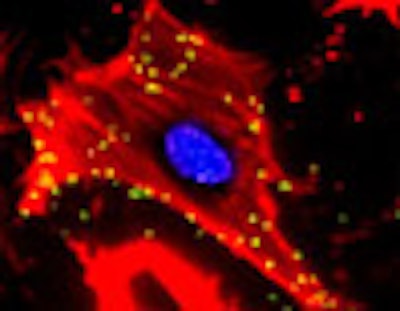
There are also new techniques for LV functional measurement, including myocardial strain, defined as a dimensionless index of the change in length of the myocardium. Its measurement may offer a "pure" index of regional LV function, but has been difficult to measure, according to Thomas.
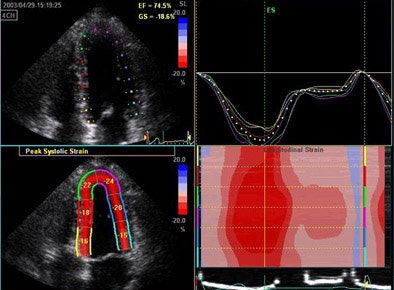 |
| 3D echocardiography measures longitudinal strain in a normal volunteer. |
"This has previously been derived using tissue Doppler, looking at the change in velocity over space and integrating it over time," he said, showing images from a patient with -20% strain indicating fiber shortening in the long axis. Strain measurements showed a strong correlation with invasive systolic function and end-diastolic pressure measurements as well.
Still, "strain is more than just a number, it's a complex mathematical tensor that linear components that stretch in three dimensions," Thomas said, including linear strain and sheer strain, which can be followed by monitoring clusters of speckles. In one example, low-level exercise showed an increase circumference of strain in a normal volunteer from -16% to -25%. "This can now be integrated in three planes to give us the wall motion rank," Thomas said. Greenberg et al demonstrated that the Doppler-derived myocardial systolic strain rate is a strong index of LV contractility (Circulation, January 2002, Vol. 105:1, pp. 99-105).
| Longitudinal strain depicted with speckle tracking in a patient recently post aortic valve replacement. Having trouble viewing this clip? Click here to view full size clip or to change format. |
Velocity vector imaging is another approach to speckle tracking that can provide offline data for strain and strain rates. It's another tool that few clinicians have now, but will soon be using more often, according to Thomas.
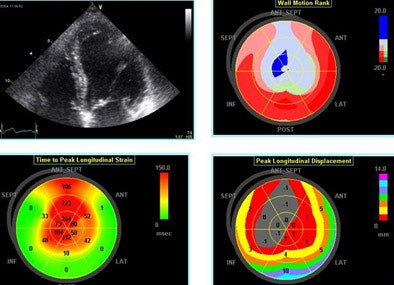 |
| Echo software demonstrates (clockwise from upper right) wall motion rank, time-to-peak longitudinal strain and peak longitudinal displacement in a patient with an LAD infarct. |
Left ventricular torsion is a potentially important measurement that can be performed with 2D speckle tracking, or with Doppler tissue imaging per Notomi et al, whose results were well-correlated to MRI measurements (Circulation, March 8, 2005, Vol. 111:9, pp. 1141-1147).
| Apical rotation shown with speckle tracking at rest (above) and with low-level exercise (below). Having trouble viewing this clip? Click here to view full size clip or to change format. |
The spiral architecture of the left ventricle produces base-apex torsion, which stores energy in systole that is released in diastole as suction, Thomas explained. Though important in LV mechanics, LV torsion has been difficult to measure.
"In next five years we will find a way to track speckles in 3D," he said. "It's very complex but it will allow us to get full strain tensor out of the myocardium as 3D density of data improves, and computer operating systems become more and more powerful."
Not to forget contrast, which can be used right now. Although LV opacification is well-established, it is "still underused in all of our practices," Thomas said. "Contrast needs to be used more frequently in echocardiography." In a stress exam, contrast opacification can spell the difference between trying to discern "a polar bear in a snowstorm," from clear images showing "a perfectly normal response to dobutamine," Thomas said of one example.
Contrast perfusion echocardiography is another important near-term goal, in which the clinician can see microbubbles accumulate in the myocardium, destroy them with a high-intensity blast of ultrasound, and watch them wash back in.
"The faster they come back the faster the perfusion, and we can do this baseline and post either adenosine or persantine, and really show good correlation with coronary stenosis," Thomas said.
Comparing myocardial contrast echocardiography (MCE) with Tc-99m single-photon emission computed tomography (SPECT), Senior et al found "better detection of relatively mild coronary stenoses with echo compared to SPECT," Thomas said (American Heart Journal, June 2004, Vol. 147:6, pp. 1100-1005).
A study this year by the same group found very good correlation between the transmurality of echo contrast to late-enhancement gadolinium-enhanced MRI. The transmural extent of infarction is an excellent predictor of long-term improvement in contractile function (American Journal of Cardiology, June 15. 2006, Vol. 97:12, pp. 1718-1721).
Targeted imaging is another exciting area. Microbubbles, which are able to adhere to activated endothelial cells, show a rather dramatic increase in adherence with anti-ICAM-1 (endothelial cell inflammatory marker intercellular adhesion molecule 1) antibodies in acclimated cells, Thomas said, citing Weller et al, who used this avidity to diagnose transplant rejection (Circulation, July 2003, Vol. 108:2, pp. 218-224).
Rupturing microbubble contrast for drug delivery is also very promising. Its use for the delivery of drugs is also very promising in that drugs can be delivered to specific organs with almost no uptake outside the targeted tissues. Mukherjee et al were able to induce angiogenesis with drug targeting (Journal of the American College of Cardiology, May 2000, Vol. 35:6, pp. 1678-1686).
Bekeredjian et al reported that "ultrasound-mediated destruction of microbubbles directs plasmid transgene expression to the heart with much greater specificity than viral vectors and can be regulated by repeated treatments. This noninvasive technique is a promising method for cardiac gene therapy," they wrote (Circulation, August 2003, Vol. 108:8, pp. 1022-1026).
Finally, the International Space Station (ISS) ultrasound project may soon get off the ground again. The launch of space shuttle Atlantis, anticipated for September 6 or 7 if there are no further delays, is aimed at ending the space station's long construction hiatus following the 2003 Columbia disaster. Eventually National Aeronautics and Space Administration (NASA) telemedicine experiments in the ISS will be able to continue -- so stay tuned for echocardiography in space.
"The main thing we're hoping out of this current mission is that it will get construction moving forward (on the ISS) so that we can get a three-man and hopefully, ultimately, a seven-man crew, which would allow much more detailed research to go on with the (ultrasound) machine," Thomas told AuntMinnie.com.
Thomas is working with NASA on the project. Practically speaking, he said, the modality would be hard to replace in space.
"You won't be seeing an MRI magnet on the space shuttle anytime soon," Thomas said.
By Eric Barnes
AuntMinnie.com staff writer
August 31, 2006
Related Reading
Spatiotemporal image correlation, TUI show promise in fetal echocardiography, August 8, 2006
Novel real-time 3D echo quantifies LV dyssynchrony, August 18, 2005
Echo illuminates prognosis in infective endocarditis, ACS, July 15, 2005
Praise for 3D echo-guided beating-heart surgery in atrial defect closure, April 13, 2005
Cardiac resynchronization therapy sharply improves survival in heart failure, March 8, 2005
Copyright © 2006 AuntMinnie.com