Breast imagers might want to board the WhoBUS, but should consider letting the THI bandwagon go by if their goal is lesion identification and/or characterization, according to two separate studies.
First, researchers from the University of Chicago shared their preliminary experience with an automated whole-breast ultrasound device (WhoBUS). In the second study, researchers from Korea and the U.S. compared tissue harmonic imaging (THI) to conventional sonography.
WhoBUS
Despite its whimsical, Dr. Seuss-like nickname, automated whole-breast ultrasound (WhoBUS) is a serious contender as a clinical tool for diagnostic workup and as a second-look tool in patients with multiple lesions in the same quadrant.
Dr. Richard Schmidt and colleagues at the University of Chicago in Illinois performed a preliminary evaluation of a WhoBUS device developed by a division of Philips Medical Systems of Andover, MA. Presented at the 2006 RSNA meeting in Chicago, the study was funded by Philips, and co-author Rob Entrekin is an employee of Koninklijke Philips Electronics.
For this study, 20 patients with 20 known lesions that were visible on handheld ultrasound (HHUS) were included. There were nine malignancies and 15 benign lesions confirmed by pathology, mammography, HHUS, or MRI.
Traditional sonography was done on an HDI5000 unit (Philips Medical Systems) with a 50-mm probe. The WhoBUS system is a hybrid mammography unit and an ultrasound scanner. It utilizes a modified mammographic compression gantry that stabilizes the breast, Schmidt said. The "high degree of automation" drives the L12/5 ultrasound probe over preset field sizes. This gantry is then connected to the ultrasound scanner with a display device.
According to the results, the mean size of malignancies based on HHUS was 19 mm, while the mean size of benign lesions was 11 mm. WhoBUS showed 100% of the malignant lesions, but found less than half of the benign lesions, most likely because the latter were smaller in size.
However, WhoBUS did spot two cancers that were not found on the original HHUS scan. In addition, the lesions that WhoBus could not detect were subtle and would have been difficult to find even with regular sonography, Schmidt noted.
The sensitivity of WhoBUS came in at 82% for malignancies and 50% for benign lesions (versus 91% sensitivity for HHUS). The smallest cancer found with WhoBUS was 4 mm.
"How do things look (on WhoBUS)? They aren't necessarily as sharp as they are on freehand ultrasound, and (WhoBUS) depends on the view orientation with the transducer and the distance from the transducer," Schmidt said.
Schmidt stressed that WhoBUS is still in the early stages of evaluation and that studies with a larger patient population are needed. Some of the difficulties that his group encountered with WhoBUS included breast slippage because of the gel, patient motion, and limited visibility at the chest wall and nipple. Also, there was restriction in scan direction for the craniocaudal view.
Nonetheless, once WhoBUS is fine-tuned, the reduction in operator dependence will make it a powerful tool, Schmidt told AuntMinnie.com. For example, the fact that WhoBUS can provide a 3D image of the breast is something that HHUS could never accomplish, he explained.
In a separate study, researchers at the Elizabeth Wende Breast Clinic in Rochester, NY, had particular success with automated breast ultrasound in dense breasts. Schmidt said that his group's patient population was too small to come to a similar conclusion, but that he expected "automated scanning to be good in all but predominantly fatty breasts."
THI
While Schmidt and other researchers continue to work out the kinks in automated breast ultrasound, radiologists from Korea and the U.S. focused their attention on more advanced techniques in traditional sonography. Unfortunately, newer didn't necessarily equal better in their study, which compared conventional ultrasound and tissue harmonic imaging (THI) in solid breast masses.
"The use of tissue harmonic imaging helps to reduce many of the artifacts that occur during conventional US, such as side-lobe, clutter, and reverberation artifacts, and improves the signal-to-noise ratio," wrote Dr. Joo Hee Cha and colleagues from Boramae Municipal Hospital as well as several other institutions in Seoul. Co-author Dr. Jeong Mi Park is from the University of Iowa in Iowa City (Radiology, January 2007, Vol. 242:1, pp. 63-69).
The group sought to determine whether THI results would affect the final diagnostic assessment of lesions and allow for better patient selection for biopsy.
For this study, 88 patients with 91 solid breast masses were examined. The majority was BI-RADS 4 (65%) and benign (67%), including fibroadenomas (31 cases). Infiltrating ductal carcinomas (24 cases) made up the majority of malignant masses. All masses seen on ultrasound were either confirmed with histopathology or with ultrasound-guided core-needle biopsy.
Conventional ultrasound and THI were done with a 5-31 MHz transducer (Logiq 700, GE Healthcare, Chalfont St. Giles, U.K.). During THI, the beam was emitted at a center frequency of 6 MHz and was received at a center frequency of 12 MHz, the authors explained.
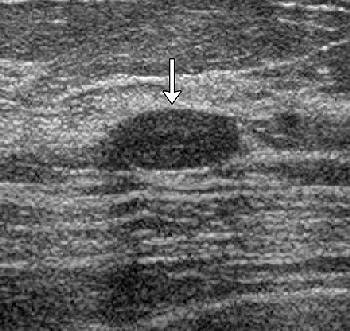 |
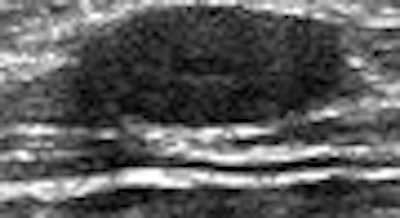
| Transverse images of fibroadenoma obtained in a 35-year-old woman during (a) conventional US and (b) tissue harmonic imaging. (a) A 1.0-cm oval-shaped slightly hypoechoic mass (arrow) is seen. (b) The mass (arrow) appears more hypoechoic and the circumscribed margin is clearly delineated. The final assessment by all readers was "probably benign" at both conventional US and tissue harmonic imaging. |
 |
| Figure 4. Cha JH, Moon WK, Cho N, et al. "Characterization of benign and malignant solid breast masses: Comparison of conventional US and tissue harmonic imaging." Radiology 2007: 242(1): 63-69. |
The 91 conventional scans and 91 THI scans were randomized, divided into two groups, and read by three readers who described lesion shape, margin, echogenicity, echotexture, posterior acoustic transmission, lesions boundary, and final BI-RADS assessment. Technique and interobserver agreement was calculated using κ statistics, along with sensitivity and specificity. A receiver operating characteristic (ROC) was performed.
According to the results, the readers description of echogenicity was most discordant (κ = 0.205) for the two ultrasound techniques. With traditional sonography, interobserver agreement was fair for orientation (κ = 0.314) and echogenicity (κ = 0.344).
"Of the 29 lesions that were described as having isoechoic echogenicity at conventional US, 27 were described differently by at least one reader at (THI)," the authors explained.
Finally, for the final assessment of solid breast masses, moderate to substantial agreement was found between the two techniques. In addition, diagnostic sensitivity was not significantly different among the readers. The overall Az value for conventional ultrasound was 0.88, while THI came in at 0.84.
The results for both traditional ultrasound and THI were as follows:
|
||||||||||||||||||||||||||||
THI did not dramatically improve the readers' ability to characterize solid breast masses as benign or malignant, nor did it significantly alter management decisions, the authors concluded. They pointed out that two current limitations of THI include reduced penetration and extensive refractive shadowing in the dense breast.
"Further improvement in (THI) is needed to increase tissue penetration, frame rate, and spatial resolution," they wrote.
By Shalmali Pal
AuntMinnie.com staff writer
February 6, 2007
Related Reading
Automated breast US proves to be sensitive screening tool in dense breasts, November 29, 2006
Streaming US, elastography US give clearer picture of breast lesions, November 16, 2006
Breast surgeon expresses reservations about screening US, May 13, 2006
Breast ultrasound experts share pearls and pitfalls, October 2, 2003
Copyright © 2007 AuntMinnie.com