A dynamic display method for subharmonic ultrasound imaging may offer considerable added value in detecting breast cancer, according to research published in the August issue of the Journal of Ultrasound in Medicine.
In their small pilot study, researchers led by Jaydev Dave of Thomas Jefferson University (TJU) Hospital in Philadelphia found that this display technique had a higher area under the receiver operator characteristics (ROC) curve than a variety of other ultrasound imaging methods. It also even outperformed mammography.
"Dynamic [cumulative maximum intensity subharmonic imaging] images in conjunction with grayscale ultrasound and [subharmonic imaging] may have the potential to improve diagnosis of breast cancer as compared to using grayscale ultrasound or [subharmonic imaging] data alone," the authors wrote (J Ultrasound Med, August 2010, Vol. 29:8, pp. 1177-1185).
Following up on earlier TJU work demonstrating the potential of subharmonic imaging in breast lesions, the research team sought to examine if cumulative maximum intensity imaging could improve the technology's efficacy. With cumulative maximum intensity imaging, a single image of a vascular structure is presented through maximum intensity projection capture of pixels over consecutive imaging frames, according to the group.
Static cumulative maximum intensity subharmonic imaging yields a composite image summarizing blood flow over multiple frames using the maximum intensity projection technique, while a dynamic mode depicts the gradual inflow pattern of the contrast agent in blood vessels, according to the researchers.
To compare the two methods with other breast imaging techniques, the researchers performed contrast-enhanced subharmonic imaging on 14 women. Scans were conducted using a modified Logiq 9 scanner (GE Healthcare, Chalfont St. Giles, U.K.) that was transmitting at 4.4 MHz and receiving at 2.2 MHz.
Baseline scans of grayscale ultrasound and power Doppler imaging were performed after mammography. The researchers also provided contrast-enhanced power Doppler imaging and regular grayscale subharmonic imaging after contrast agent administration; six patients received 0.5 mL of Optison (GE), while eight had 0.25 mL of Definity (Lantheus Medical Imaging, North Billerica, MA).
Grayscale subharmonic imaging was performed after a second contrast dose was administered (4.0 mL of Optison or 1.4 mL of Definity) following a 15-minute interval.
All patients received a core biopsy for histopathologic assessment following ultrasound. To reduce noise and blurring and compensate for motion artifacts, the researchers deployed a new automated motion compensation algorithm for both imaging modes.
After an initial phase of the study established the optimal threshold for the automated algorithm, a radiologist with more than 17 years of breast imaging experience compared the imaging techniques. Blinded to mammographic and pathologic findings, the radiologist evaluated the ultrasound clips on a six-point scale ranging from 0 (no lesion) to 5 (malignant findings).
Over a 2.5-year period and with at least a three-month interval between each review session, the radiologist reviewed the images in the following order:
- Standard grayscale
- Standard grayscale and precontrast power Doppler imaging
- Standard grayscale and contrast-enhanced power Doppler imaging
- Standard grayscale and subharmonic imaging
- Standard grayscale, subharmonic imaging, and static cumulative maximum intensity subharmonic imaging
- Standard grayscale, subharmonic imaging, and dynamic cumulative maximum intensity subharmonic imaging
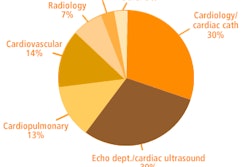
The area under the ROC curve (which shows the incremental value for each modality) for diagnosing breast cancer for each method were as follows:
- Grayscale: 0.64
- Power Doppler imaging: 0.64
- Contrast-enhanced power Doppler imaging: 0.67
- Mammography: 0.76
- Subharmonic imaging: 0.78
- Static cumulative maximum intensity display mode for subharmonic imaging: 0.75
- Dynamic cumulative maximum intensity display mode for subharmonic imaging: 0.90
The higher area under the ROC curve for the dynamic cumulative maximum intensity display mode over mammography was statistically significantly (p = 0.03).
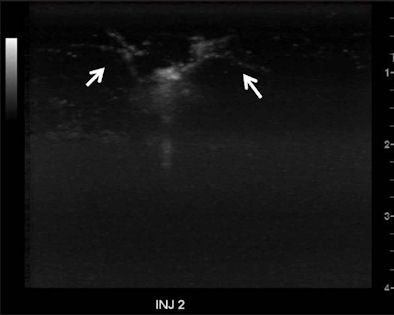 |
| Cumulative maximum intensity subharmonic breast ultrasound images show detailed tumor microvasculature (arrows). Image courtesy of the Journal of Ultrasound in Medicine. |
In other findings, the combination of standard grayscale, subharmonic imaging, and dynamic cumulative maximum intensity subharmonic imaging had a sensitivity of 100%, specificity of 50%, accuracy of 63%, positive predictive value of 40%, and negative predictive value of 100%.
In comparison, mammography alone had a sensitivity of 100%, specificity of 20%, accuracy of 38%, positive predictive value of 27%, and negative predictive value of 100%. Standard grayscale ultrasound and precontrast power Doppler imaging both turned in 50% sensitivity, 92% specificity, 81% accuracy, 67% positive predictive value, and 85% negative predictive value.
Standard grayscale ultrasound and postcontrast power Doppler imaging had 75% sensitivity, 75% specificity, 75% accuracy, 50% positive predictive value, and 90% negative predictive value. The combination of standard grayscale ultrasound and subharmonic imaging yielded 75% sensitivity, 83% specificity, 81% accuracy, 60% positive predictive value, and 91% negative predictive value.
The authors noted that their long-term goal is to demonstrate that dynamic cumulative maximum intensity subharmonic imaging can help characterize breast lesions by showing composite vascular tumor morphology.
"The improved detection with dynamic [cumulative maximum intensity subharmonic imaging] calls for a larger clinical trial for this technique before implementing it in a clinical environment," the researchers concluded. "The technique may then be used as an adjunct to mammography and standard ultrasound, which may increase the specificity of breast cancer characterization (consistent with one of the goals of the U.S. Preventive Services Task Force in updating their recommendation in 2009 for biennial breast screening examinations)."
In discussing the study at last month's American Association of Physicists in Medicine (AAPM) meeting in Philadelphia, co-author Flemming Forsberg, PhD, said that the group has received funding from the U.S. National Institutes of Health (NIH) to conduct a large-scale, four-year trial at two centers with the goal of including data from 450 women.
"So we can try to prove -- or disprove, for that matter -- that this technique will work on a relevant patient population size," he said.
By Erik L. Ridley
AuntMinnie.com staff writer
August 5, 2010
Related Reading
Conn. breast density law causes conundrum for mammo sites, April 29, 2010
Inexperienced readers benefit most from breast US CAD, March 5, 2010
Color Doppler US predicts survival of breast cancer patients, January 26, 2010
Fuzzy 3D ultrasound CAD sharpens breast cancer sensitivity, September 3, 2009
Subharmonic breast imaging technique shows potential, May 26, 2006
Copyright © 2010 AuntMinnie.com