Ultrasound elastography can be a valuable adjunct to conventional ultrasound in preoperative assessment of axillary lymph nodes, according to research from the Cambridge Breast Unit in Cambridge, U.K.
In a 50-patient study, the study team found that elastography could reliably demonstrate axillary lymph nodes and differentiate between benign and malignant nodes. When used in conjunction with conventional ultrasound, elastography could also increase sensitivity for identifying abnormal lymph nodes for biopsy, said presenter Kathryn Taylor.
She presented the findings during a scientific session at the 2011 European Congress of Radiology (ECR), held earlier this month in Vienna.
In women with suspected breast cancer, axillary lymph nodes are typically examined using ultrasound with or without core biopsy. But this routine practice carries a significant false-negative rate, Taylor said.
"Up to 30% of nodes appearing as normal node morphology are actually metastatic," she said.
As a result, the researchers sought to compare the use of elastography with conventional ultrasound in the axilla. They aimed to determine if the technique could demonstrate axillary lymph nodes at all, whether it could differentiate benign from malignant nodes, and whether it could -- in conjunction with conventional ultrasound -- increase sensitivity for identifying abnormal lymph nodes.
In the pilot patient cohort, 50 women with sonographically suspicious (BI-RADS category 4 or 5) solid breast lesions received elastography of the ipsilateral axilla at the same time as their conventional ultrasound. Scans were performed using a Sonix SP scanner (Ultrasonix Medical) with an 8- to 16-MHz transducer and a frame rate of more than 10 frames per second. The patients had an age range of 27 to 88 years, with a mean age of 57.
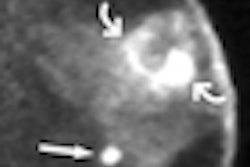
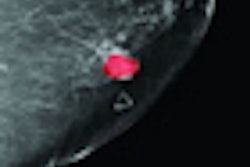
The researchers utilized Cambridge University's own Stradwin software, which displays elastograms in grayscale alongside the conventional ultrasound studies. A black color display denotes stiff tissue, while white represents soft tissue.
Conventional ultrasound studies were scored using standard criteria, while the elastography studies were visually scored in retrospective fashion as 1 (normal), 2 (benign), 3 (suspicious), or 4 (malignant). A score of 1 indicated that the node tissue was indistinguishable from surrounding tissue, while a score of 2 indicated there was an incomplete or complete rim on the outside of the node.
A score of 3 was given if more than 50% of the node was displayed as black (or stiff) on the software, and a score of 4 meant that the tissue was shown as completely black. The researchers set a theoretical cut point for biopsy between scores 2 and 3.
The researchers then compared the elastography results with the conventional ultrasound findings and the reference standard of surgical histology.
Of the 50 patients, 21 (42%) had metastatic axillary lymph nodes, while 29 (58%) had normal nodes.
|
In the 23 studies that were reviewed as positive on conventional ultrasound, 19 were also positive on elastography. Of the 19 that were also positive on elastography, 15 were ultimately confirmed positive on histology, Taylor said. An additional four positive results were found on elastography alone.
Four of the studies reported as positive on conventional ultrasound were negative on elastography. Three of these negative results were also negative on histology, while one negative was ultimately positive on histology.
On elastography, 23 patients had negative results that were ultimately confirmed to be negative on histology. One was a false negative, however.
"We need to remember in this scenario [that] unlike elastography of breast lesions where we are in principle more interested in specificity than sensitivity since we don't want to perform unnecessary benign biopsies, in the axilla, within reason, we are more interested in sensitivity," she said.
At the expense of lower specificity, higher sensitivity could also be achieved if the elastography cut-point for biopsy was changed to be between BI-RADS score 1 and score 2, according to Taylor.
"In practical terms, [this] would make it a very easy decision whether or not to biopsy, because we would then be biopsying basically anything in the node area that looks stiff," she said. "That would actually give us a sensitivity of 100% and a specificity -- still acceptable -- of 66%."