CHICAGO - Positron emission mammography (PEM) is more specific than breast MRI for presurgical planning of the ipsilateral breast in women with breast cancer. And this specificity could mean fewer unnecessary biopsies, researchers report.
The study, conducted by Wendie Berg, MD, PhD, of the American College of Radiology Imaging Network (ACRIN) in Lutherville, MD, and colleagues, was presented at the 2010 RSNA meeting on Monday.
The group found that PEM had greater specificity than breast MRI at the breast and lesion levels. The two technologies had comparable breast-level sensitivity, although breast MRI had greater lesion-level sensitivity and more accurately depicted the need for mastectomy. The research has also been published online in Radiology (November 12, 2010); it was funded in part by Naviscan (San Diego), the manufacturer of the PEM device used.
Between September 2006 and November 2008, 472 women with newly diagnosed breast cancer who had been offered breast-conserving surgery participated in the study, undergoing both bilateral contrast-enhanced MRI and FDG-PEM in random order. Of the total cohort, 388 completed the study. The median tumor size was 1.5 cm.
The exams found additional cancers in the alternate breast in 82 women, or 21% of the study cohort, Berg told session attendees. The median tumor size of these additional cancers was 0.7 cm. Of the additional cancers:
- 28 (34%) were found with both PEM and breast MRI
- 21 (26%) were found with breast MRI only
- 14 (17%) were found with PEM only
- 7 (8.5%) were found with mammography and ultrasound
- 12 (15%) were missed by all imaging exams
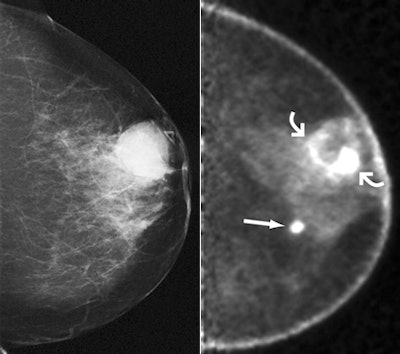 |
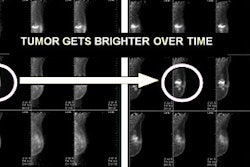
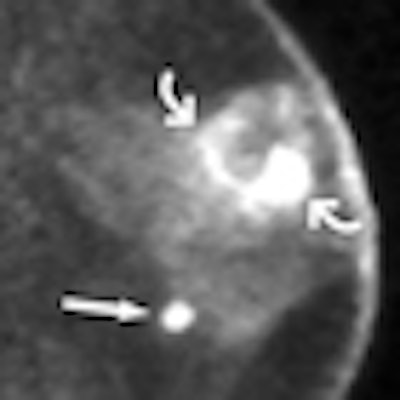
| Images obtained in 68-year-old woman who previously underwent right mastectomy for cancer and was noted to have lump in left breast. (above, left) Lump was shown to correspond to 2.8-cm indistinctly marginated mass (triangular marker) on craniocaudal mammogram. Ultrasound-guided core-needle biopsy revealed grade III invasive ductal carcinoma (IDC). (above, right) Craniocaudal and (below, left) mediolateral oblique PEM images (5.6-mm section thickness) obtained beginning 70 minutes after intravenous injection of 10.4 mCi (384.8 MBq) of FDG show intense rim uptake in known cancer (curved arrows). Approximately 5 cm medial and inferior to this region, intense FDG uptake was noted in second, 1-cm mass (straight arrow). |
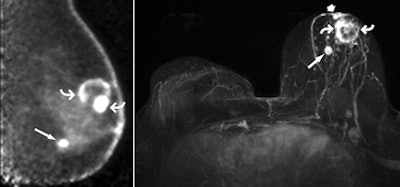 |
| (above, right) Axial maximum intensity projection of left breast subtraction of precontrast images from 3D spoiled gradient-echo T1-weighted MR images obtained 90 seconds after intravenous injection of 0.1 mmol of gadoversetamide per kg of body weight also shows rim enhancement in known malignancy (curved arrows) and intense enhancement in second, 1-cm mass (long straight arrow) in lower inner region of breast. Metastatic axillary nodes were suspected at MR imaging. The patient opted for direct mastectomy; histopathologic analysis confirmed multicentric grade III IDC, the largest of which was 3.0 cm. The second mass was confirmed to be 1.2-cm grade III IDC with a less than 5% ductal carcinoma in situ component. A third 0.7-cm grade III IDC (straight short arrow) noted in the immediate retroareolar region was difficult to distinguish from normal nipple enhancement but visible on both PEM and MR images. Two of five sentinel nodes showed metastatic disease. Both PEM and MR imaging correctly depicted multicentric disease that was not seen at mammography. All images courtesy of RSNA. |
Combining PEM and breast MRI increased cancer detection to 61 (74%) of 82 breasts, compared to 49 (60%) of 82 breasts identified with MR imaging alone. Of the 306 women without additional cancer, 279 (91.2%) were correctly assessed with PEM, compared to 264 (86.3%) who were correctly assessed with MR imaging. And results improved even further when the investigators had access to prior mammography or ultrasound results: another reason for collaboration, according to Berg.
"If nuclear imaging is going to take hold in breast [applications], we have to involve our breast imagers in the process," she said.
Biopsies prompted by PEM data had a higher positive predictive value than those prompted by breast MRI: 47 (66%) of 71 cases versus 61 (53%) of 116 malignant lesions that were imaging positive. Fifty-six (14%) of the 388 women required mastectomy: 40 (71%) of these women were identified with MR imaging, and 20 (36%) were identified with PEM. Eleven (2.8%) women underwent unnecessary mastectomy, which was prompted by only MR findings in five women, by only PEM findings in one, and by PEM and MR findings in five.
Accuracy at the breast level was similar across the modalities at 80.7% for MRI and 82.7% for PEM, Berg told attendees.
"Yes, PEM was more specific than MRI, but because it had a lower lesion-level sensitivity, the overall accuracy between the two modalities was the same," she said.
For women who cannot tolerate breast MRI, PEM is now a proven alternative in surgical planning, Berg said. And although MRI was slightly more sensitive to the extent of disease, PEM was less likely to prompt unnecessary biopsies. But for the biopsies that do need to be performed, be sure to have the proper support, Berg said.
"If PEM is offered at your center, it's best to also offer PEM-guided biopsy, as 17% of the cancers in our study were seen only with this technology," she concluded.
By Kate Madden Yee
AuntMinnie.com staff writer
November 30, 2010
Related Reading
MBI three times as effective as mammo in dense tissue, November 16, 2010
MBI casts wider net for improved breast cancer diagnosis, September 14, 2010
MBI could help breast centers caught in economic squeeze, September 14, 2010
Radiation dose in women's imaging: Are we scared yet? September 14, 2010
Nuclear breast imaging may have greater cancer risks, August 24, 2010
Copyright © 2010 AuntMinnie.com