Particular breast cancer characteristics contribute to AI-mammography misses -- and radiologists should keep them in mind when using the technology with mammography, according to a study published June 24 in Radiology.
These characteristics include luminal cancers, dense breast tissue, nonmammary zone locations, architectural distortions, and amorphous calcifications, wrote a team led by Ok Hee Woo, MD, of Korea University Guro Hospital in Seoul.
"Although AI is useful for detecting advanced-stage invasive cancers, it is inadequate for identifying cancers with some of the features revealed in this study," the group noted. "Understanding the features of AI-missed invasive cancers on mammograms can help readers use AI appropriately in clinical practice, thus contributing to its further optimization."
AI has come to be regarded as a promising tool for helping read mammograms, but it can still miss breast cancers, Woo and colleagues wrote. Few studies have evaluated AI-read mammography's false-negative rate in invasive cancers, and the "clinicopathologic and radiologic features of AI-missed invasive cancers and reasons for missing cancers remain underexplored."
The group investigated the false-negative rate of AI mammograms by molecular subtype (hormone receptor–positive [luminal] vs. human epidermal growth factor receptor 2 [HER2]-enriched vs. triple-negative) and tracked the features of and reasons for these missed cancers. The team's study included 1,082 women diagnosed with 1,097 cancers between January 2014 and December 2020.
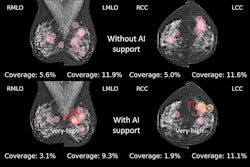
A commercial AI software was used to read the mammograms (Lunit Insight MMG). AI-missed cancers were defined as "those for which AI did not identify a precise location matching the reference standard." Three radiologists, blinded to whether breast cancer had been missed by AI-mammography, classified any cancers as either "actionable" or "under threshold"; readers aware of AI-missed cancers determined reasons for the misses in a further review.
AI missed 154 of 1,097 cancers (14%). These missed cancers had the following characteristics:
- They were found in younger women.
- Tumor size was less than or equal to 2 cm.
- They had a lower histologic grade and fewer lymph node metastases.
- More of them were categorized as BI-RADS 4.
- The cancers had lower Ki-67 expression and fewer nonmammary zone locations.
Of the AI-missed cancers, 61.7% were actionable, the researchers found. Further reasons for the misses included dense breast tissue (n = 56), nonmammary zone locations (n = 22), architectural distortions (n = 12), and amorphous microcalcifications (n = 5).
Regarding the false-negative rate, the team also reported the following:
AI mammography's false-negative rate by breast cancer subtype* | |
Type of breast cancer | False-positive rate |
| HER2-enriched | 9% |
| Luminal | 17.2% |
| Triple-negative | 14.5% |
| *All results statistically significant | |
 Images in a 42-year-old asymptomatic woman. (A) Digital mammograms show an irregular spiculated mass in the left upper outer quadrant (arrows). (B) Artificial intelligence (AI) software did not mark this lesion due to a low abnormality score. (C) Ultrasound and (D) breast MRI scans revealed a 1.1-cm irregular mass in the left upper outer breast at the 1-o'clock position. Breast-conserving surgery was performed; the lesion was confirmed as a 1.1-cm invasive ductal carcinoma (luminal subtype, histologic grade 3) without axillary lymph node metastasis. The lesion was classified as actionable; three radiologists categorized it as suspicious. The reason for the AI miss was that the lesion was obscured by overlying dense breast tissue. CC = craniocaudal, MLO = mediolateral. Images and caption courtesy of the RSNA.
Images in a 42-year-old asymptomatic woman. (A) Digital mammograms show an irregular spiculated mass in the left upper outer quadrant (arrows). (B) Artificial intelligence (AI) software did not mark this lesion due to a low abnormality score. (C) Ultrasound and (D) breast MRI scans revealed a 1.1-cm irregular mass in the left upper outer breast at the 1-o'clock position. Breast-conserving surgery was performed; the lesion was confirmed as a 1.1-cm invasive ductal carcinoma (luminal subtype, histologic grade 3) without axillary lymph node metastasis. The lesion was classified as actionable; three radiologists categorized it as suspicious. The reason for the AI miss was that the lesion was obscured by overlying dense breast tissue. CC = craniocaudal, MLO = mediolateral. Images and caption courtesy of the RSNA.
In an accompanying editorial, Lisa Mullen, MD, of Johns Hopkins University School of Medicine in Baltimore, urged radiologists using AI with mammography to "pay close attention to dense breasts and nonmammary zone areas, as well as search carefully for architectural distortion, microcalcifications, and small lesions."
"When using AI, it is critical for radiologists to understand what could be potentially missed by the software so that [they] can use the information to decrease the chance of missed cancers," she concluded.
The complete study can be found here.