AuntMinnie.com presents the fourth in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of this modality.
Fellow UltraSounder,
Ob/gyn applications are the pre-eminent and all-around best technical expressions of diagnostic ultrasound, likely accounting for more daily studies than all other ultrasound tasks combined. However, this area is also underutilized or inappropriately utilized and often relegated to a screening rather than diagnostic role.
 |
| Dr. Jason Birnholz. |
In the earliest days of ultrasound, this form of imaging was used as a way of avoiding ionizing radiation exposure. The choice was never made because of the information content of the images, and there was often a sentiment that radiation methods were somehow more valid for patient care decisions. This notion became even more exaggerated when CT scanning ironed out its initial problems.
Think of ultrasound as a pictorial mapping of the type, distribution, and arrangement of collagen in the imaging field (or a map of the spatial distribution of the modulus of elasticity). This information correlates with cellular histology and is distinct from that provided on an atomic scale of x-rays and in the small molecular scale of MRI; it is captured without ionizing radiation exposure, in real-time and without the need for sedation, immobilization, or discomfort, all of which is especially relevant to fetal and gynecological evaluations.
There is a persistent reliance among primary care physicians on the traditional physical exam for diagnostic triage. That is, referrals for ultrasound may be limited to the times someone thinks they feel something odd in a bimanual pelvic exam or when there is a size and date discrepancy in estimated uterine size in pregnancy. The physical exam is a set of tools that have evolved out of clinical necessity, but, unfortunately, these lack the sensitivity or specificity for early detection of pathology deep to the skin surface.
However, manual physical exams have a distinct advantage in that the examiner is always integrating information as the exam progresses, revising the differential diagnosis as information is accrued. For example, the impression is channeled one way in a young, sexually active woman with adnexal tenderness, fever, and leukocytosis and another direction in an asymptomatic elderly woman with vaginal spotting or unintentional weight loss.
The new percussion
Ultrasound is a modern version of the physical exam technique of percussion. To be most informative, an ultrasound exam is conducted as a manual physical exam with hypothesis testing and diagnostic refinement as imaging progresses. Most of its diagnostic power is lost when exams consist of a series of static images, referred for interpretation after the imaging is concluded. In an outpatient setting without access to electronic medical records, there may not even be basic clinical information about the patient to supplement the history that the examiner can elicit at the time of the study.
The first type of ultrasound unit to diffuse into general use was the "bistable mechanical scanner," which had a single-element transducer attached to a jointed, rigid metal arm that constrained the scan to a line path. Images were black and white without any grayscale variations, mainly showing the borders of some organs. There was an A-mode display of signal amplitude by which one could distinguish cysts and other simple fluid collections from "solids" by estimating signal attenuation.
Each image took a relatively long time to form, and scans frequently had to be redone with alternate instrument settings, which was also true with early "grayscale" display instruments in the mid-1970s, although information retrieval was improved. A lot of the early ultrasound physician explorers came to rely on technologists who could devote the time necessary to obtain a complete image set, freeing them to concentrate on the interpretation phase of the study.
The hybrid digital/analog high-speed array scanners with mobile handheld transducer arrays of the early 1980s revolutionized ultrasound in terms of its clinical applications. While it made the integrative physical exam form of ultrasound practical, the operational trend of technologist acquisition of specific information had already been established.
Expanded use
During the next decade, physically small and mobile, low-cost, and lower-performance equipment became widely available, and ultrasound was "liberated" from the need for expert or specialized supervision. Any practice could, if they wished, buy equipment, buy a technologist, or hire a mobile service and start to ultrasound patients.
This approach made some form of ultrasound available in a relatively brief time to most pregnant women, one of the most explosive growth patterns experienced in any form of medical imaging. But, the price was miring ultrasound into a set of habits (and biases) from an earlier time in the development of the method.
Something interesting and unique happened in the early days of the obstetrics takeover: the notion of the "Level I exam." The name has changed to protect the guilty, but the concept persists and flourishes and by now may even be part of the so-called "community standard."
For the first time in the history of medicine, a group of physicians admitted publically that it was ethically and (they hoped legally) permissible to do an incomplete or limited patient examination, just by saying upfront that for many patients that is all they needed.
I suppose there is some rationale to that concept if you are the only care provider in a remote location, but how can that translate to an urban center teeming with specialists, or when there is an expert facility within a different department in the same hospital or clinic or a freestanding facility right down the block? It seems like a misapplication of truth in advertising to medical practice now after many years of clinical usage and several generations of equipment development.
Thinking about exams and procedures
Many facilities involved in women's healthcare seem quick and unafraid to take on the responsibility of a fetal exam, but they hesitate or refuse to do gynecologic ultrasound. The fetal exam is probably the most difficult type of ultrasound study; there is an entire body with all of its separate systems to evaluate. Diagnostic concerns involve anatomy, physiology, pathology, behavior, functional maturation, and growth, and everything changes weekly through pregnancy. Besides, there is the placenta, the uterus (including the cervix), and by extension almost anything maternal that can impact the pregnancy. The target regions for gynecologic exams are the uterus, ovaries, some support structures, and the bladder; there is a limited range of pathology.
The first thing we do when an adult female patient comes to our facility is to send her to the washroom. An empty bladder is best. There has never been a point to having a full bladder after about 12 weeks of pregnancy, when you can couple into the uterus above the pelvic brim, transabdominally, about 95% of the time. I've visited facilities where late-pregnancy women were writhing on the table because they were given large volumes of water to drink quickly and then nearly all of the scanning took place above the bladder. It is true that prior to the mid 1980s, when imaging was almost exclusively transabdominal, bladder filling was necessary for accessing the ovaries and the uterus when it was in a mid- to retroverted position or for locating an embryo in an early gravid uterus. But that was then. Endovaginal transducers have been available and in routine use for more than 20 years. We always need to be re-evaluating how and why we do ultrasound exams.
Endovaginal scanning
Endovaginal scanning is essential because there are fewer and thinner layers to traverse between the probe and the uterus and ovaries than is ever the case with transabdominal viewing; noise is vastly lower when imaging through this portal.
The relative improvement in image quality is most striking for low-performance equipment that doesn't have noise suppression. Because targets are usually close to the probe at the vaginal apex, very high frequencies can be used for exquisite spatial and contrast resolution. If you cannot or prefer not to do endovaginal scanning, then you should not be doing pelvic ultrasound. This is a really important point. It is absolutely disrespectful of any patient to undertake the responsibility of a medical diagnostic exam with the knowledge that the study may be flawed or incomplete for any reason.
There are good reasons for endovaginal scanning all throughout pregnancy. The first trimester is obvious, but afterward, if the head presents, it's the best way to see the brain. If the breech presents, then the lower spine and pelvic viscera will be visualized optimally, and in all cases, this is the absolute best way to evaluate the cervix and premature delivery potential associated with cervical softening and shortening.
Except for very slender women, 15 to 16 weeks is the very worst time in pregnancy to do an anatomic survey. Fetuses tend to be too deep for transabdominal viewing and too high up for complete endovaginal imaging. Earlier and later are both better.
We always have the patient self-insert the probe, which is well-lubricated with a slippery gel. Contrary to a common bias, suspected or real placenta previa is an indication for endovaginal viewing, because it lets you assess the relation of the placenta and marginal vessels to the internal os directly.
An endovaginal transducer will not pass into a normal cervix, and should the cervix be fully effaced, which is pretty rare without labor, that will be obvious from viewing during probe insertion. There is scarcely ever a reason why endovaginal scanning should not be done in an adult woman with a suspicion or potential for serious conditions.
A magical screening sign
Nuchal thickness has evolved as some kind of magical screening sign since it began to be popularized around 1990. The early protocols utilized transabdominal viewing and, astonishingly, many facilities cling to this clinically unsustainable practice.
There are two forms of nuchal subcutaneous abnormality, both deriving from problems with cervical lymphatics including the thoracic duct. When venous pressure is high or thoracic duct drainage is physically compromised, there is a smooth, lengthy elevation of skin behind the neck. Some of these cases have aneuploidy, and, no surprise, a significant percentage of those with normal karyotyping have structural or functional cardiac disease.
In looking endovaginally, most of the cases with diastolic heart failure will also have tiny pleural, pericardial, or intraperitoneal effusions that are not perceived transabdominally, classifying them as "hydrops." There is a second form of nuchal regional abnormalities resulting from occlusions or spotty absence of lymphatics in the neck proximal to a patent thoracic duct. This results in lymph pockets or cystic hygromas that vary from a few, small collections in the neck to multiple tiny to large collections scattered over the back, neck, and scalp.
Cystic hygromas have a higher likelihood of aneuploidy than the smooth large elevation of nuchal skin; small collections are often impossible to see transabdominally, especially with low-performance equipment and/or with an obese patient. It seems a lot better to utilize available higher-resolution imaging for this kind of survey than to try to improve the accuracy of limited transabdominal ultrasound by combining it with a series of equally insensitive maternal blood assays.
Do no harm
The famous advice: "Try to help, but above all, do no harm," comes from the first aphorism of Hippocrates; it is thoroughly ingrained in medical education and practice. I was puzzled a few years ago when some obstetrical ultrasound practitioners seemed to be invoking Hippocrates by asserting that endovaginal Doppler should be avoided in pregnancy, especially with endovaginal acquisition in the first trimester.
We might choose to forget that there had been a long history of using hours of continuous-wave Doppler with a transducer anchored over a fetal chest for heart rate monitoring in late pregnancy and to neglect the singular lack of any evidence of harmful effects of pulsed Doppler in the literature.
My bewilderment was mainly because in low-power mode, the peak power of pulsed Doppler for most commercial systems I have used is 60 mW/cm2, well below the arbitrary standard of 100 mW/cm2 for B-mode imaging. If a few seconds of Doppler with a handheld probe (minute probe movements prevent wave concentration) is so bad, how could you do any B-mode imaging at all with its higher power level?
To be sure, ultrasound dosimetry is a very complicated subject and safety is always a concern. Newer devices monitor the mechanical and thermal indices of various instrument settings, enabling the operator to minimize whatever potential risks might be associated with mechanical, nonionizing radiation.
The mechanical index (MI) concerns pressure effects and the potential for cavitation, which is improbable at diagnostic ultrasound power levels in tissues devoid of air bubbles. The thermal index (TI) concerns the potential for temperature rise within tissues, which is more likely in highly absorbent structures like bone and of least concern with water density fields (like amniotic fluid and isodense early embryos).
If you don't do embryo or fetal Doppler, chances are you won't think of using it for the nongravid uterus or ovaries either. The mindset in radiology for at least the past 60 years is the assumption that there is always a potential biological hazard to everything -- each exposure should be as brief and as low in energy transfer as practical without sacrificing image quality, to the point where no adequate information can be obtained. The principle of dose minimization is known internationally as ALARA (as low as reasonably achievable). Appearing often in CT reports, ALARA is applicable to all forms of radiant-energy imaging.
Risk of bypassing ultrasound
When considering a theoretical risk of radiant energy exposure, it's always important to estimate the actual risk to the patient from not doing a study; that is, how management may suffer by not having the information that might have been obtained from that specific exam.
With this in mind, let's think a little about endovaginal Doppler. Endovaginal imaging enables the use of higher transducer frequencies for imaging and for Doppler, because attenuation and scatter are less than with long transabdominal scan paths.
Doppler backscatter from moving ensembles increases with the fourth power of frequency (which is the Tyndall effect and the reason why downshifting headlight frequency is helpful in night driving in fog). The consequence is that modest increases in frequency lead to much greater Doppler sensitivity, enhancing characterization of tissue motion and blood flow.
A Doppler tracing is usually depicted as a frequency shift (which is directly proportional to target velocity) versus time. It is easy to think of this kind of continuous line tracing as a kind of electrocardiogram, but it is really different in that the waveform reflects the mechanics of flow, the pump efficiency of the heart, and the compliance of the vascular network.
For early embryos, heart rate is the most precise indicator of conceptual age; depressed rate, arrhythmias, and variations in the Doppler waveform all predict impending demise, whereas a normal Doppler pattern is highly predictive of pregnancy continuation.
Myometrial hyperemia
In gynecologic exams, 2D Doppler makes it easy to identify or exclude myometrial hyperemia. In most instances this coincides with adenomyosis, which has a much higher prevalence than is suggested by the preultrasound literature. Increased vascularity in the endometrial boundary zone accounts for the shorter, more intense, and often painful periods with clots that many parous women experience in their early 40s.
Myometrial hyperemia results from epidermal growth factor I that is elaborated by some fibroids, and it has been identified (angiographically) as associated with recurrent implantation failure in infertility patients. 2D Doppler also provides a graphic way to identify a potential bleeding site when a patient with submucous myomas or endometrial polyps presents with menorrhagia.
Doppler information is essential in sorting out the issue of pelvic venous congestion, which is like a hormone-driven equivalent to the gravitational dynamics of varicose veins in the legs. I have selected these examples rather than hyperemia with inflammatory disease or neovascularity with tumors because they apply to the vast majority of pelvic ultrasound studies in healthy women requested due to menstrual irregularities or pelvic pain.
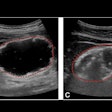
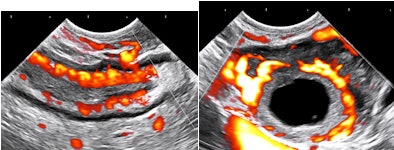
Let's have a look at some selected images from a recent study of a 30-year-old woman with uncertain dates and a positive pregnancy test:
 |
 |
| All images courtesy of Dr. Jason Birnholz. |
There is a intrauterine pregnancy with a (right) corpus luteum with an intact vascular margin. A regular heart rate of 122 beats per minute implies a 6.0-week stage. The Doppler pattern has separate filling and ejection phases. The decidual boundary is thick and well implanted. But there was another unexpected finding when looking at the left ovary:
 |
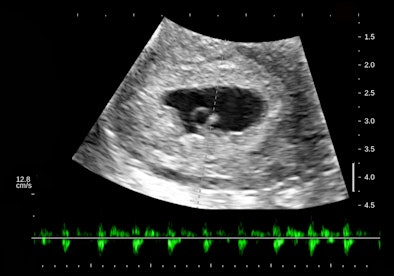 |
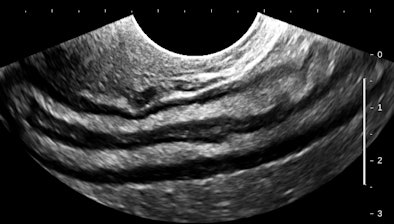 |
The findings in these views of the distal descending left colon are typical and classic for active ulcerative colitis. The submucosa is thick, reflective, and hyperemic. Some divots can be seen along the mucosa and one transverse section shows a tiny submucosal cyst. What do you think a transabdominal exam would have shown? Would that study have served the best needs of this patient?
Moving forward
Every facility needs to establish exam protocols that reconcile the needs and best interests of patients with its personnel and equipment, and all individuals involved in the diagnostic ultrasound process needs to think about how they can achieve their personal best for every examination.
I think it's now time to abandon the ethically flawed notion of different levels of exam for any aspect of women's imaging and seek to provide uniformly complete studies for everyone. At the same time, it behooves all of us to make full use of the ultrasound capabilities that we have and update equipment and technique as often as practical.
I am certain that obstetrical and gynecologic applications are the topic areas where ultrasound can continue to expand and provide uniquely valuable contributions to medical care.
Dr. Jason Birnholz is a graduate of Johns Hopkins School of Medicine and did his diagnostic radiology residency at Massachusetts General Hospital. He was awarded an Advanced Academic Fellowship from the James Picker Foundation and has been a professor of radiology.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.