The combination of a novel, operator-independent ultrasound therapy device and tissue-type plasminogen activator (tPA) therapy may be able to increase the rate of artery recanalization in patients with ischemic stroke, according to a study published online October 24 in Stroke.
In phase II results from the Combined Lysis of Thrombus in Brain Ischemia With Transcranial Ultrasound and Systemic tPA-Hands-Free (CLOTBUST-HF) study, tPA therapy followed by sonothrombolysis yielded higher rates of sustained complete recanalization in patients with ischemic stroke caused by proximal intracranial occlusion, compared with historical rates of recanalization achieved from tPA alone.
"Our goal is to open up more arteries in the brain and help stroke patients recover," said Dr. Andrew Barreto, lead author and assistant professor of neurology in the stroke program at the University of Texas Health Science Center, in a statement. "This technology would have a significant impact on patients, families, and society if we could improve outcomes by another 5% to 10% by adding ultrasound to patients who've already received tPA."
The study was sponsored by the U.S. National Institutes of Health (NIH) and conducted at the University of Texas Health Science Center and the University of Alabama at Birmingham (Stroke, October 24, 2013).
A promising adjunct
Only 20% to 30% of acute stroke patients achieve complete recanalization within two hours of receiving intravenous tPA therapy, according to the authors. Furthermore, up to one-third of those with any recanalization experience reocclusion.
Sonothrombolysis represents a safe and promising adjunct to tPA, but delivery via cranial bone windows requires training for both anatomic localization and waveform recognition.
"Thus, mass expansion of properly trained technicians or clinicians to provide 24/7 stroke coverage to complete a pivotal clinical trial of sonothrombolysis represents a major hurdle," wrote the research team.
As a result, the researchers performed a phase II trial of a hands-free, operator-independent device (ClotBust-ER, Cerevast Therapeutics). Developed through industry and NIH funding, the unit employs 2-MHz pulsed-wave ultrasound technology and delivers energy through both temporal windows and the suboccipital window via 18 separate transducers.
The researchers enrolled 20 patients at two stroke centers. The patients, 60% of whom were men, had a mean age of 63 and a median NIH Stroke Scale score of 15. In 14 (70%) of the 20 patients, pretreatment occlusion was present in the middle cerebral artery. Pretreatment occlusion was also found in the terminal internal carotid artery in three patients (15%) and in the vertebral artery in three patients (15%).
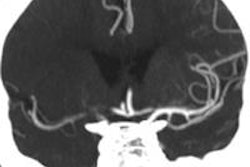
After receiving standard-dose intravenous tPA and shortly after tPA bolus, all patients were given a two-hour therapeutic exposure to 2-MHz pulsed-wave ultrasound using the ClotBust device. All subjects also received pretreatment and post-treatment transcranial Doppler ultrasound or CT angiography.
The primary outcome measure was occurrence of symptomatic intracerebral hemorrhage. The researchers collected NIH Stroke Scale scores at two hours and a modified Rankin Scale score at 90 days.
At the beginning of sonothrombolysis, the median time to tPA was 22 minutes. The researchers reported that all patients tolerated the entire two hours of insonation; no one developed symptomatic intracerebral hemorrhage. In addition, no serious adverse events were related to the study device, according to the authors.
Higher recanalization rate
Of the 20 patients, eight (40%; 95% confidence interval: 19%-64%) achieved complete recanalization after two hours, while two (10%; 95% confidence interval: 1%-32%) had partial recanalization. By specific occlusion type, middle cerebral artery occlusions had the highest complete recanalization rate, at eight of 14 (57%; 95% confidence interval: 29%-82%).
Overall, five patients (25%, 95% confidence interval: 7%-49%) had a modified Rankin Scale score of 0 to 1 after 90 days.
The researchers acknowledged limitations of their study, including a small sample size that may make it difficult to draw reliable conclusions. In addition, there was the possibility of selection bias, and investigators were unblinded to patient treatment.
Nonetheless, high-frequency delivery of transcranial sonothrombolysis in combination with intravenous tPA seems potentially safe in patients with proximal intracranial arterial occlusions and may produce more complete recanalization than tPA alone, the authors concluded.
"Further study of this treatment combination seems warranted and is ongoing in a phase III efficacy trial," they wrote.