The U.S. Preventive Services Task Force (USPSTF) has finalized its draft recommendation advising against the use of widespread ultrasound screening for asymptomatic carotid artery stenosis (CAS) as a tool for stroke prevention.
In an article published online July 8 in the Annals of Internal Medicine, the task force reported on its review of the literature. The low prevalence of carotid artery stenosis would result in many false positives on screening ultrasound, the group concluded.
What's more, a large number of surgical interventions such as carotid endarterectomy (CEA) could be performed that aren't any better than standard medical therapies such as statins in terms of reducing stroke risk, according to the task force. The findings prompted the task force to maintain a D rating, meaning it recommends against the procedure and discourages its use.
Preventing stroke risk
The goal of CAS screening is to reduce the risk of stroke, which affects 7 million U.S. adults each year, with ischemic strokes accounting for nearly 90%. Carotid artery stenosis has an estimated prevalence of 1%, but it causes some 10% of ischemic strokes, according to USPSTF.
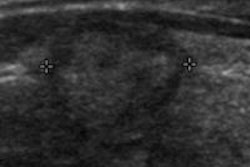
Screening ultrasound could potentially reduce the risk of stroke by enabling healthcare providers to detect it earlier and deploy interventional strategies such as CEA or stents to clear plaque and restore blood flow. But medical therapies such as statins and antihypertensive agents have already been effective in reducing stroke rates over the past few decades, USPSTF noted.
Indeed, in 2007 the task force gave CAS screening with duplex ultrasound a D rating. Even so, many surgical procedures and medical interventions based on CAS scans continue to be performed, and "free or 'cash-on-the-barrel' screenings are offered in public locations across the [U.S.]," the authors wrote.
To update its 2007 recommendation, the task force sought to assess current evidence on whether screening reduces the risk for ipsilateral stroke, and on any harms associated with screening and interventions for carotid artery stenosis. The group evaluated current evidence on the incremental benefit of medical therapy and on risk-stratification tools.
After developing an analytic framework and key questions to guide the review, the task force searched Medline, the Cochrane Library, and Embase for English-language articles published through September 2013. The authors also performed a targeted update search of Medline for trials published through March 31, 2014, and they searched clinical trial registries for unpublished literature. The reference lists of included studies and literature suggested by reviewers were also considered.
The review included 78 published articles that reported on 56 studies, according to the task force. However, the group did not find any eligible studies that provided direct evidence on whether screening reduced ipsilateral stroke.
Asymptomatic CAS has a low prevalence in the general adult population, and noninvasive screening with ultrasonography would result in many false-positive results due to an average specificity of 92% for detecting 60% or greater stenosis, according to the authors.
"If externally validated, reliable risk-stratification tools were available to distinguish subgroups of persons who were more likely to have CAS, then the ratio of true-positive results to false-positive results would improve," they wrote. "However, the only study that attempted external validation of such a tool found inadequate discrimination."
Hard to estimate benefit
The task force said that it's difficult to obtain an accurate estimate of potential benefit for the current primary care population by comparing CEA to medical therapies. There is a wide variety of medical therapies for stroke reduction, and the clinical studies examined often didn't clearly define or standardize the therapies used. Some studies didn't include treatments now considered to be standard, including aggressive management of blood pressure and lipids.
The new Carotid Revascularization Endarterectomy Versus Stenting Trial 2 (CREST-2) is set to begin later this year, the authors noted. It will compare the combination of carotid angioplasty and stenting (CAAS) and medical therapy versus medical therapy alone, as well as the combination of CEA and medical therapy versus medical therapy alone.
In theory, patients at greater risk for ipsilateral stroke may be more likely to benefit from surgery or intervention; however, the task force didn't find any validated and reliable risk-stratification tools that can identify those with asymptomatic CAS who are at lower or higher risk for stroke or those who are at greater risk for harms from CEA or CAAS.
"One may expect that persons with greater reduction of the carotid diameter would have greater potential for benefit, but subgroup analyses from trials that compared CEA with medical therapy found no significant difference by CAS percentage," they wrote.
It's possible that many of the studies had a lack of reporting or underreporting of some harms, the task force wrote.