Ultrasound-guided injections of platelet-rich plasma (PRP) for rotator cuff tendinopathy can delay degenerative changes of the tendons and yield quantifiable pain relief and functional improvement, Italian researchers found.
In a retrospective study of 240 patients, researchers led by Dr. Francesco Arrigoni of the University of L'Aquila in L'Aquila, Italy, found that ultrasound-guided PRP injection of the supraspinatus tendon significantly outperformed the use of medical and physical therapy alone.
"Intratendinous injection of PRP can modify the natural history of the rotator cuff tendinopathy compared with medical and physical therapies," said Arrigoni, who shared the group's findings during a scientific session at the RSNA 2014 meeting in Chicago.
PRP has been increasingly used in recent years to treat musculoskeletal injuries such as tendinopathy. While a number of studies have assessed the effectiveness of the therapy, researchers have primarily evaluated the clinical symptoms and functions of the treated patient. Furthermore, the studies have produced ambiguous and sometimes conflicting results, Arrigoni said.
As a result, the Italian team sought to evaluate the effectiveness of ultrasound-guided PRP injection of the supraspinatus tendon and compare it with medical and physical therapy alone. Patients were included in the study if they had a diagnosis of tendinosis or a focal tear of the supraspinatus tendon with a diameter of 1 cm or less. The researchers evaluated the success of each method based on morphological changes as seen on MRI and four years of follow-up.
Half of the 240 patients in the study were treated with ultrasound-guided PRP injection, while the other half received only medical and physical therapy. The hospital's blood transfusion department prepared the PRP. After being given local anesthesia with mepivacaine hydrochloride in the subacromial bursa, patients received one of two PRP injections under ultrasound guidance in the supraspinatus tendon. The second injection was provided 21 days later. Patients were immobilized with a soft brace for three days after injection.
Patients with a history of trauma or surgery during the four-year follow-up period were excluded, Arrigoni noted. MRI exams were performed on each patient before and four years after PRP injection, as well as on the group of patients who received medical and physical therapy.
Based on the MRI results, patients were classified as showing improvement, having stationary findings, or worsening. In addition, all patients were given a clinical and functional evaluation before therapy and after the four-year follow-up period. Pain was assessed using scores based on a visual analogue scale (VAS), while shoulder joint function was evaluated with Constant function scores.
| MRI results after 4 years | |||||
| Improvement | Stationary findings (no change) | Worsening | |||
| Patients receiving US-guided PRP | 31.7% | 48.3% | 20% | ||
| Patients who had only medical and physical therapy | 3.3% | 34.2% | 62.5% | ||
| Clinical and functional evaluation results after 4 years | |||||
| Improvement in pain levels (as measured by VAS scores) | Improvement in shoulder joint function (as measured with Constant function scores) | ||||
| Patients receiving US-guided PRP | 74.5% | 56% | |||
| Patients who had only medical and physical therapy | 16.2% | 9% | |||
"PRP injection in fact delays the degenerative changes of the tendons, and this is documented by the pain relief and functional improvement," Arrigoni said.
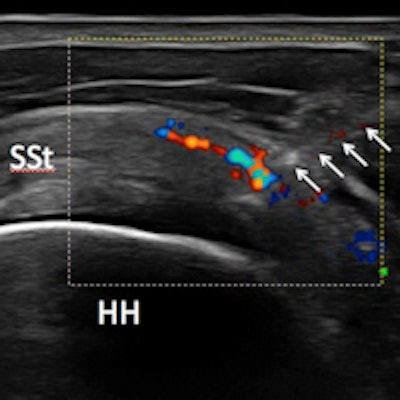
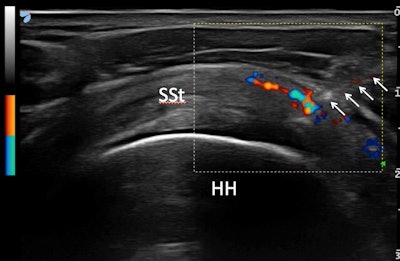 Ultrasound-guided injections of PRP in the supraspinatus tendon. Needle is shown with arrows and the spread of PRP is visible on color Doppler. All images courtesy of Dr. Francesco Arrigoni.
Ultrasound-guided injections of PRP in the supraspinatus tendon. Needle is shown with arrows and the spread of PRP is visible on color Doppler. All images courtesy of Dr. Francesco Arrigoni.Arrigoni noted that MRI findings provide important evidence of the therapy's effectiveness, serving to confirm the clinical evidence.
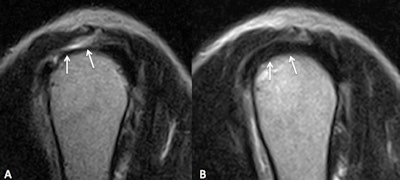 Sagittal T2-weighted MR images of the shoulder. Focal lesion (arrows) is shown on left (A). Image taken two years later (B) shows evidence of healthy rotator cuff tendon.
Sagittal T2-weighted MR images of the shoulder. Focal lesion (arrows) is shown on left (A). Image taken two years later (B) shows evidence of healthy rotator cuff tendon.He acknowledged a number of limitations to the study. Patients were not divided by age, and the medical and physical therapy was not standardized. In addition, the researchers did not quantify the degree of improvement or worsening of the tendinopathy on imaging, he said.