
AuntMinnie.com presents the 23rd in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of the modality.
As I like the notion of bringing diagnostic ultrasound to patients, I was impressed by a new portable, battery-operated, apparently full-featured ultrasound unit at the RSNA 2014 meeting. Out of interest and also as a potential buyer, I decided to evaluate ultraportable equipment options.
This article covers new, upgraded, or replacement equipment in general, along with some technical fundamentals that some people new to the field may not know. What I am after is a unit for a wide range of clinical applications, with performance equivalent to my own fixed-position office equipment, just much smaller. I did not include any units over 2 lb weight in my assessment, and I wanted U.S. Food and Drug Administration (FDA) clearance for immediate clinical use.
A moral issue
 Dr. Jason Birnholz.
Dr. Jason Birnholz.I always look at promotional materials, but I need to have hands-on time before I make any decision. Sometimes the images are high-quality under ideal circumstances, but that can be misleading. The most basic decision is this: Does comparative image quality justify its use on patients?
Equipment acquisition is much more of a moral issue than an economic one. Cost-benefit analyses are fine for population-based decision-making, but their application to individuals is somewhat problematic. For whatever diagnostic task or application area, we are all obligated to do as well as we can absolutely, not just as well as the equipment might be able to perform. Equipment selection should not be the quality-limiting step in the delivery of diagnostic ultrasound services.
I always start with a phantom. I practice with the controls and take the time to assure myself of basic image quality. If you do not have a commercial phantom at hand, you can make a good one with gelatin and Metamucil using the recipe reported by Bude and Adler. I'm fond of pickles, olives, and cherries as targets within the gel. You won't notice any distortions related to sound propagation velocity with this phantom at room temperature. I never scan people until I am satisfied by the phantom imaging stage.
A 'retro' concept
The earliest ultrasound units were entirely analog devices. The clinical expansion of our field was synchronous with and dependent upon the digital revolution in computing and electronics.
One of the innovative concepts in this emerging field is the brainchild of Dr. John McKinnon, an academic radiologist in Santiago, Chile, and a former president of the Chilean Society of Radiology. His handheld unit is distinct in not having a central processing unit (CPU). I'd like to be able to say "charmingly retro," but that would be incorrect, since our early analog device precursor has been reimagined with self-programming digital circuitry. Its name is Taote, which means "physician" in the Easter Island native language.
Vader Johnson, chief engineer for developer Airson Labs, brought me a prototype Taote unit from Santiago so I could take a look. Because it hasn't received FDA clearance, I limited scanning to a phantom. I thought I should include it in my analysis anyway because of its unique design and what I learned from Vader.
One of the things I look for is that cystic voids are echo-free throughout and that they have sharp borders. That is, that there are no side-lobe or grating lobe artifacts. This prototype seemed to do that very well, even with an off-the-shelf, 3.5-MHz curved-array transducer from a Chinese manufacturer.
I asked Vader why the company, alone as far as I knew, had decided to avoid using a CPU. He said it was to get less noise and better tissue fidelity without high power consumption. He went on to explain that in digital computers, operations occur at clocked intervals. The best way to reduce digital noise in a computer system is through redundancy, which means making the clock speed (and the number of operations per unit time) as fast as possible; this is power intensive.
The Airson plan is to do the analog-to-digital conversion near to the transducer and then operate digitally thereafter. The company dissected all the programmed computer operations in B-mode ultrasound and implemented them as hardwired circuits with field-programmable gate array (FPGA) components.
The result is a compact, instant-on imaging system with long battery life. The limitation, perhaps, is a loss of flexibility. That is, the system may be dynamite for a set of scanning conditions or a particular application, but it may not necessarily have a wider or more general use. A few basic controls were built into the test system, and I presume further attention to this point will be part of the next stage of development.
The display
 Vader Johnson of Chilean handheld ultrasound developer Airson Labs. All images courtesy of Dr. Jason Birnholz.
Vader Johnson of Chilean handheld ultrasound developer Airson Labs. All images courtesy of Dr. Jason Birnholz.Vader is wearing a pair of virtual reality (VR) glasses that were donated to the project. They provide a reasonably bright conventional TV image. Vader said that Airson liked the idea of maximum portability, but that there were other display options.
Personally, I really dislike the notion of VR glasses, although I never had a chance to test Google Glass in this kind of application. Patients having a diagnostic exam are always apprehensive, and anything that dehumanizes the examiner must be avoided.
I have always found that a big part of educating patients (and obtaining relevant history) comes from being able to point out things on a screen during the exam. If a patient needs to embark on a therapeutic journey with an uncertain, albeit hopeful, destination, they need to be clear about the evidence for the diagnosis.
Even for minor forms of pathology, visual evidence leads to better drug and treatment compliance. This is the main reason why I also do not like small-screen displays, especially conventional video ones. The other is that I cannot see much detail. We have reached the time when high-definition TV should be a minimal requirement for image-based electronic devices.
Array transducers
The first commercial ultraportable ultrasound unit I tested was a "wobbler," harking back to the mechanical sector scanners of the late 1970s. Those devices did a pretty good job for their time, mainly because they used circular-faced single elements with an aperture big enough for the beam profile to hold together for a reasonable distance within tissue. The few new mechanical units in the ultraportable realm tend to use newer quartz-family transducer materials that have lower power requirements for pulse formation. However, they do not seem to be as efficient as receivers, a drawback that leads to excessive noise.
This device did not pass the phantom part of the testing, but I wanted to mention it because it is important to understand why "modern" multifunctional ultrasound units need to use array transducers (which actually has nothing to do with avoiding the wear and tear of moving parts). The answer has to do with the exquisite control of the properties of the acoustic pulses on transmit and receive that can be achieved electronically.
Early phased arrays used control of timing of excitation for beam steering and for listening for returns along that same beam path. They also tended to use acoustic lenses to minimize off-axis insonification. One of the problems of early array systems was "cross-talk," or signals leaking between elements, that contributed significantly to noise. This has been addressed by new transducer materials, and by the way that arrays that are fabricated.
Registering transmit and receive beam patterns makes it possible to use various forms of electronic pulse coding to get special results. This is a little like encrypting a message so that only a designated person can receive it.
By now, I would assume that most of you know about chirp signals. These are pulses that are long in time and go from low to high frequencies continuously. Returns can be decoded electronically to an equivalent for a pulse that is very short in time with higher energy. This is a way to achieve high-frequency imaging for a much greater depth and with a lower peak energy exposure burden than you would get otherwise. If you look up "orthogonal Golay codes" you will find one of the common techniques of pulse coding for noise reduction.
Prepublication review
I also unsuccessfully requested demo equipment from two large, multinational companies. One was a small-screen device with a novel transducer and the other uses an Asus tablet computer with a curved 3.5-MHz array transducer, marketed for obstetrical use.
Both of these units appeared to have been disregarded at RSNA 2014 by attendees, as well as the companies' representatives. I interviewed the person in charge of mobile ultrasound from the first company about two months ago. He told me that the company had seen such potential in the ultraportable market that they had purchased the Scandinavian company that had originally developed their device.
He expressed surprise that a radiologist would have any interest in the equipment and thought that it would have its greatest impact in the emergency room and in primary care, particularly in India. I expressed my interest in evaluating a unit and thought that even if performance were limited, there would be applications in interventional radiology for needle guidance or catheter placement.
The company was not willing to demo a unit, but they would send me one if I signed an agreement with a section that mandated that I receive their approval before publishing or saying anything about the unit. I had a similar experience with the second vendor, who also would not send me a demo unit without being able to review anything I might say about it.
I presume you will all immediately appreciate the outrage this provoked with its flagrant neglect of academic or journalistic impartiality. The large equipment vendors may not understand that we, as responsible medical users of equipment, rely on honest and trustworthy peer-to-peer information exchanges. You may not agree with anything I write in this column, but you should have no doubt that I am expressing myself with integrity, just as I would interact with a patient. I have nothing commercial to declare.
Controls, controls
I mentioned earlier about using a phantom to become familiar with system controls. I have heard a sentiment from salespeople about various kinds of small units to the effect that there are no controls, so that anyone could use the product out of the package. All you needed to do was select a preset for the part of the body you are looking at and your worries about scanning will vanish. To be sure, most ultraportables do not have a lot of screen space for controls, so their absence is sometimes portrayed as a virtue, especially for anyone with knobophobia.
Unfortunately, patients are not standardized. The paradox is that the amateur scanner needs the highest-quality images to make sense of what they show and to know when a finding is real and not spurious. Ultrasound is both operator- and equipment-dependent.
I have never been a fan of presets. I've talked to a lot of engineers developing ultrasound equipment, and the notion I hear is the misconception that there are a few tissues and a massive number of diseases. So they set up presets more or less based on anatomy instead of trying to cope with all kinds of diseases. What we need is to identify and stage pathology and pathophysiology. There are really only a few processes, such as inflammation, edema, cellular infiltration, neoplasia, and fibrosis, and they each tend to look much alike wherever they occur.
Most manufacturers of "high-end" systems cite presets as a starting point that everyone should modify as needed. However, this seems not to be the case with ultraportables, as potential settings are limited to factory defaults, labeled anatomically. The more flexibility one has in adjusting the equipment, the better you can do for every patient you see and not just the fat-free models that tend to appear for product demos.
The right device
I also found an ultraportable in the low-rent district of the RSNA 2014 exhibit halls. I know nothing about what the RSNA charges vendors, but there are back and peripheral locations of the floor that are not heavily frequented, where technically innovative start-ups may be found.
My attention was grabbed by Sonoscanner, a French company that had a thin, lightweight tablet with a high-definition display and capabilities for B-mode, M-mode, and pulsed- and color-flow Doppler. The system, called U-Lite, utilizes harmonics. There was a 2- to 6-MHz curved array; an 8- to 16-MHz linear array; and, introduced since last year, a high-frequency endovaginal array transducer. I was sent curved-array and linear-array units and I will have the endovaginal array by the time you see this column.
What astounded me was that the system is fully adjustable through a mini-keyboard plugged into one of the USB connectors. There is a screen overlay for all kinds of adjustment, so that you can see the results in real-time. Preferred settings are saved by depth in any of a number of folders. My experience is that once these are set, I really did not have to vary them much afterward, although I can. The display shifts from vertical to horizontal as the unit is rotated, like a smartphone, and the image is moved or magnified with finger movements. Here are some Metamucil gelatin phantom images on my first day of scanning with the linear array at 10 and 12 MHz. These are original except for cropping.
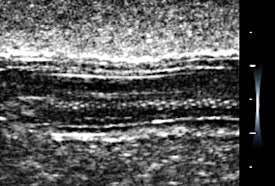 Long-axis view of a gherkin.
Long-axis view of a gherkin.The first phantom image is of a gherkin, although I should say "cornichon," as this is a French unit. The settings were optimized for spatial resolution showing the tiny seeds along the axis.
Look at the magnified cherry images below. They hold together beautifully, and there is an impressive visible grayscale intensity range. The fluid cleft and the pitted center of the cherry have sharp clear boundaries, and there is an acoustic shadow effect deep to the cherry. These settings were mainly for contrast resolution, which is the most important performance factor for recognizing and excluding pathology. I could have done better with near-field gain and I fixed that later.
 A pitted cherry.
A pitted cherry.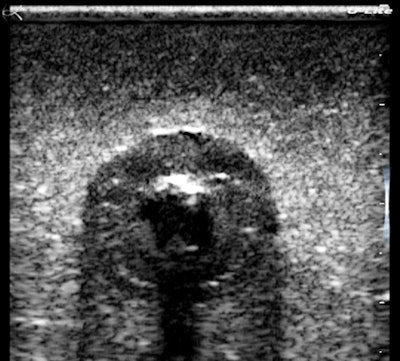 Oblique-magnified view of the cherry.
Oblique-magnified view of the cherry.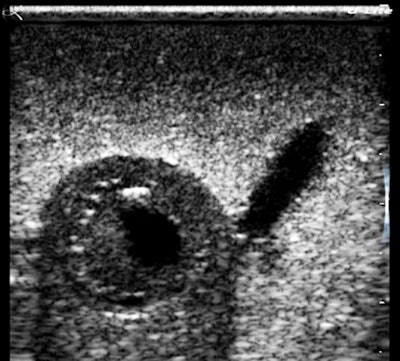 Transverse-magnified view of the cherry.
Transverse-magnified view of the cherry.The images were uploaded by Wi-Fi to an encrypted database where there are tools for annotating, measuring, or labeling images and for generating a report to be emailed out to the patient and referring physician.
This device has been very well-engineered for medical use, which is not a surprise when you learn that its originator is a radiologist, Dr. Bruno Richard, who scans patients daily in his practice. He also happens to have a doctorate in biomedical engineering from the University of Paris and is a world expert on ultrasonic transducers. When I interviewed him at RSNA 2014, I asked what he was most proud of in his long career, and without much delay he said, "the curved array."
I have been using U-Lite clinically, and I will talk about actual cases with all three transducers in the next article. The conclusion that I have been coming to is that taking a fully functional ultrasound device directly to patients or to public health venues promotes the early detection of a variety of conditions for which minimal interventions can greatly affect life span and quality of life.
It could very well be that ultraportable ultrasound devices will have a big role in mass screening applications, especially now that we have tools for communicating, archiving, and mining massive amounts of data within a local or regional healthcare system.
Dr. Jason Birnholz was one of the few advanced academic fellows of the James Picker Foundation, and he has been a professor of radiology and obstetrics. He is a fellow of the American College of Radiology and the Royal College of Radiology, and he was an associate fellow of the American College of Obstetricians and Gynecologists.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com.



















