Shear-wave elastography can noninvasively predict the presence of esophageal varices in patients with the first stage of liver cirrhosis, and bests other measures for spotting high-risk varices, according to research published in the July issue of the Journal of Ultrasound in Medicine.
In a study of more than 100 patients with compensated cirrhosis, a type of cirrhosis in which no symptoms are typically present, a South Korean research team found that shear-wave elastography produced higher accuracy than the commonly used method of platelet count/spleen diameter ratio for predicting esophageal varices, or abnormal enlarged veins in the esophagus. What's more, shear-wave elastography was the only effective independent variable for predicting high-risk esophageal varices.
"If our results are confirmed in larger prospective studies, it may be possible to reduce the endoscopic burden in the patients with compensated cirrhosis," wrote the group led by Dr. Tae Yoon Kim and Dr. Tae Yeob Kim of Hanyang University Guri Hospital in Guri-si, South Korea.
A predictor of mortality
Chronic liver disease commonly leads to liver cirrhosis and portal hypertension, which can induce esophageal varices, ascites, and hepatorenal syndrome. The presence of esophageal varices is an independent predictor of mortality, according to the group (J Ultrasound Med, July 2016, Vol. 35:7, pp. 1373-1381).
Current guidelines mandate endoscopic screening for esophageal varices in patients with chronic liver disease at the compensated stage of cirrhosis, when symptoms such as jaundice, ascites, variceal hemorrhage, or hepatic encephalopathy begin to appear. The guidelines also recommend that high-risk varices -- defined as grades F2 or F3 -- be treated with beta-blockers, and those with nonhigh-risk varices be rechecked under the routine screening protocol.
"However, these current guidelines involve a considerable endoscopic burden and financial cost," the authors wrote. "Thus, accurate noninvasive predictors of portal hypertension and esophageal varices are greatly needed."
As a result, the researchers sought to determine if shear-wave elastography could improve upon other proposed noninvasive methods such as routine biological parameters, transient elastography, the platelet count/spleen diameter ratio, and esophageal capsule endoscopy. For a secondary objective, the team wanted to compare the performance of shear-wave elastography in patients with and without splenomegaly.
The researchers analyzed 103 patients with compensated cirrhosis. Of these patients, 63 had grade F0 varices (no varicose appearance), while 27 had F1 varices (straight, small-caliber varices), and 13 had grade F2 (moderately enlarged, beady varices) or F3 varices (markedly enlarged, nodular, or tumor-shaped varices). All patients received shear-wave elastography on an Aixplorer ultrasound scanner (SuperSonic Imagine) with a SC6-1 convex broadband probe for measuring liver stiffness.
After conventional sonography was performed, liver stiffness was measured by three abdominal radiologists with six to 17 years of clinical experience in abdominal radiology and liver sonography. The radiologists were blinded to the patients' clinical and endosopic results. Endoscopy was performed by two experienced upper gastroenterologists within one month before or after the shear-wave elastography exam.
Better performance
The team calculated the optimal tissue stiffness cut-off value for predicting the presence of esophageal varices was 13.9 kPa; the optimal cut-off value for high-risk varices was 16.1 kPa. After performing receiver operating characteristic (ROC) analyses to determine diagnostic performance, the researchers found that liver stiffness (determined by shear-wave elastography) produced the highest area under the curve for both predicting esophageal varices in general, as well as specifically for high-risk esophageal varices.
| Area under the curve (AUC) for predicting esophageal varices | ||
| AUC for esophageal varices | AUC for high-risk esophageal varices | |
| Liver stiffness | 0.887 | 0.880 |
| Platelet count/spleen diameter ratio | 0.770 | 0.841 |
| Platelet count | 0.765 | 0.845 |
| Spleen diameter | 0.692 | 0.722 |
The area under the curve for liver stiffness in predicting esophageal varices in general was significantly higher than other measures, such as platelet count (p = 0.025), spleen diameter (p = 0.001), and the ratio of platelet count to spleen diameter (p = 0.027). The differences for high-risk esophageal varices were not statistically significant, however.
"Spleen size, the platelet count, and the platelet count/spleen diameter ratio may also be good predictors of large esophageal varices and severe portal hypertension," the authors wrote.
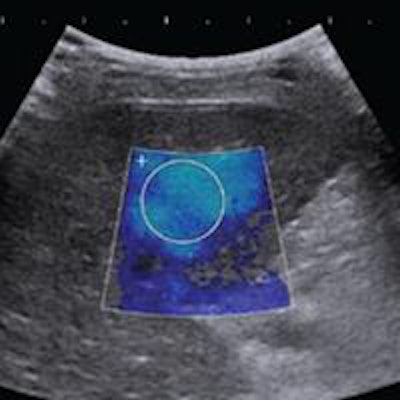
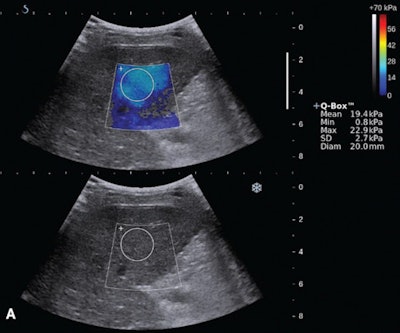 Shear-wave elastography (top) and endoscopy (bottom) of a 59-year old woman with a F2 varix. The median liver stiffness on shear-wave elastography was 19.3 kPa. Images courtesy of the Journal of Ultrasound in Medicine.
Shear-wave elastography (top) and endoscopy (bottom) of a 59-year old woman with a F2 varix. The median liver stiffness on shear-wave elastography was 19.3 kPa. Images courtesy of the Journal of Ultrasound in Medicine.In other study results, liver stiffness also yielded the highest area under the curve for predicting esophageal varices in patients without splenomegaly. The difference with platelet count/spleen diameter was statistically significant (p = 0.034) Liver stiffness also had the highest area under the curve for predicting esophageal varices in patients with splenomegaly, but that difference did not reach statistical significance (p = 0.292).
"All of the predictors are effective in predicting esophageal varices that accompany splenomegaly," the authors wrote. "Thus, this result is meaningful for the diagnostic performance of [shear-wave elastography] in early portal hypertension."
Significant predictors
Delving deeper into their data, the researchers then performed multivariate logistic regression analyses to determine if any specific patient characteristic or test result could independently predict esophageal varices.
Only two variables were found to be statistically significant predictors of esophageal varices: liver stiffness (odds ratio, 1.517; p < 0.001) and the platelet count/spleen diameter ratio (odds ratio, 0.881; p = 0.038). However, only liver stiffness (odds ratio, 1.201; p = 0.012) was a significant predictor for the presence of high-risk varices, "suggesting that liver stiffness is the only effective variable for predicting high-risk varices, although it does not have better diagnostic performance than the platelet count/spleen diameter ratio," according to the group.
The researchers acknowledged several limitations of their study, including its retrospective design and reliance on a relatively small number of patients at a single institution. There may have also been a selection bias due to the inclusion of patients with compensated cirrhosis based on chart review, according to the researchers. The study also included a patient population with diverse underlying causes for liver disease. This inhomogeneity may have reduced the areas under the curve, the team noted.