A machine-learning model that uses both ultrasound and clinicopathological features could help predict treatment success in breast cancer patients, according to research published January 21 in Ultrasound in Medicine & Biology.
Researchers from Tongji Shanxi Hospital in Taiyuan, China, reported success from the model, including achieving high accuracy in predicting pathologic complete response following neoadjuvant chemotherapy and identifying significant predictors of success from tumor data.
“These findings indicate that the model may serve as a valuable tool for efficacy evaluation,” wrote a team led by Meihong Jia and colleagues.
Numerous studies in recent years have analyzed the performance of nomograms and deep-learning models for predicting pathological complete response in treating breast cancer. Many approaches use deep-learning algorithms along with single-modal ultrasound to assess the efficacy of chemotherapy.
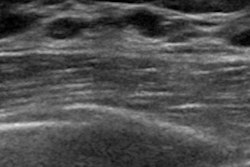
The researchers noted limited data for integrating multimodal ultrasound (ultrasound combined with shear wave elastography [SWE]) for such prediction.
Jia and colleagues developed their machine-learning model based on ultrasonography and clinicopathological features to predict pathological complete response following neoadjuvant chemotherapy for breast cancer treatment. The team’s goal included establishing a noninvasive prediction tool for individualized treatment planning.
Using a combination of imaging and clinicopathological features, the team developed seven machine learning models, including random forest, logistic regression, and extreme gradient boosting (XGBoost). It also optimized model parameters through 10-fold cross-validation.
Among the developed models, XGBoost demonstrated superior performance over all the other models. This included achieving an area under the ROC curve (AUROC) of 0.89, sensitivity of 0.81, and specificity of 0.8 in the test set.
Shapley Additive Explanations analysis identified the following significant predictors of complete pathologic response: ER-negative, PR-negative, tumor short diameter, and HER2-positive. Decision curve analysis indicated that XGBoost provided the highest net benefit within clinical decision thresholds (10% to 90%). And the calibration curve showed good consistency between predicted and observed outcomes, with a slope approaching 1 (Brier score = 0.11).
The study authors wrote that ultrasound’s accessibility and cost-effectiveness make the modality a more feasible option over MRI or CT for the dynamic monitoring of treatment response.
“After radiologists acquire conventional ultrasound and SWE data and clinicians collect basic clinicopathological feature, the XGBoost model can rapidly output the probability of pathologic complete response to neoadjuvant chemotherapy within minutes, requiring no additional specialized equipment or complex operations,” they wrote.
The investigators also called for future research to improve the model’s performance by integrating additional imaging modalities or by incorporating temporal data collected during treatment.
“This model offers a reliable approach for the early assessment of [chemotherapy] efficacy and may support the development of individualized treatment strategies,” they concluded.
Read the full study here.