
During an echo exam, the right heart is often overlooked and little attention is paid to its size, function, and prognostic implications. This article series reviews the proper methods to quantify the right heart for both size and function.
Part 1 of our series reviewed the basic anatomy of the right heart and outlined the American Society of Echocardiography's (ASE) updated recommendations for quantifying right heart size and function, while part 2 discussed proper measurements for evaluating the size of the right ventricle (RV).
 Judith Buckland, president of CardioServ.
Judith Buckland, president of CardioServ.Part 3 focused on the preferred volumetric measurement methods and linear measurements for calculating the size of the right atrium (RA), and part 4 featured our eight tips for correctly measuring tricuspid annular plane systolic excursion (TAPSE) and the S' wave (tissue Doppler imaging-derived tricuspid lateral annular systolic velocity). Another method listed by the ASE for evaluating RV function -- fractional area change (FAC) -- was the subject of part 5.
RIMP
In this article, we'll review how to use a fourth quantitative method -- the right ventricular index of myocardial performance (RIMP) -- for evaluating RV function with echocardiography. An index of global RV performance, the RIMP value represents the relationship between the ejection and nonejection time of the heart. The "nonejection" times are the very small increments of time when all heart valves are closed:
- Just after the tricuspid/mitral valve closes and before the pulmonic/aortic valves open
- Just after the pulmonic/aortic valve closes and before the tricuspid/mitral valves open again
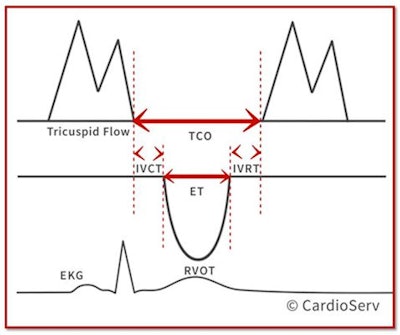
These time intervals can be visualized in the diagram below: The diagram makes it easier to appreciate that the total time the tricuspid valve is closed (TCO) is longer than the pulmonic ejection time (ET). This brings our attention to the little intervals of time before and after the right ventricular outflow tract (RVOT) ejection time when the tricuspid valve (TV) is still closed: the isovolumetric contraction time (IVCT) and the isovolumetric relaxation time (IVRT).
 All images courtesy of CardioServ.
All images courtesy of CardioServ.Note that TCO time is the time between the opening and closing of the tricuspid valve, while ET is the time during the ejection of blood through the pulmonic valve. The IVCT is the time after TV closure and before pulmonic valve (PV) opening, while the IVRT is the time after PV closure and TV opening.
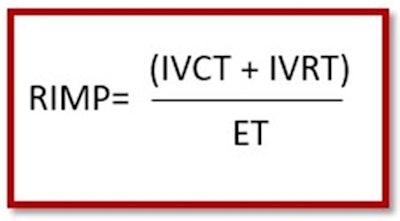
RIMP is the nonejection time (IVRT + IVCT) divided by the ET.
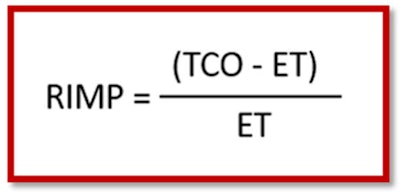
Remember, we are just trying to find a way to express nonejection time/ejection time. There's also another way of expressing nonejection time that does not require measuring the tiny time intervals of the IVCT and IVRT. Instead, we can subtract the RVOT ejection time from the TCO. In the following equation you can see the relationship between TCO and ET.
Obtaining RIMP
There are two methods for obtaining RIMP. One requires a two-step process that involves taking measurements from two different images and paying careful attention to RR intervals. Yes, I know I lost you already. Don't worry. We are not going to teach that method as we understand the reality of real-life scanning!
Instead, we will teach the tissue Doppler method with all the measurements performed on a single beat. The good news is that if you are already performing the S' wave, then you already freeze the perfect tissue Doppler image to perform RIMP.
- The ASE suggests using the standard apical 4 (AP4) window when performing RIMP measurement.
- Use the same technique used for S' wave and place the cursor over the lateral annulus of the tricuspid valve:
- Pulse-wave Doppler the tissue Doppler image (TDI)
- Decrease gains to avoid noise and limit artifacts
- Ensure the motion of the annulus is toward the apex
- Freeze image with a clear S', E', and A' waveform
- Measure all the time intervals from same one single beat:
- Tricuspid valve closure-to-open time (TCO)
- Time the tricuspid valve is closed
- From the end of TV A-wave to beginning of the following TV E-wave
- Do not get confused and measure the duration of the E-A wave. You are measuring the time in between the E-A waves!
- Ejection time of RVOT
- Represented by the duration of the S' wave
- Do not include the IVCT and IVRT times
- From the end of IVCT to the beginning of IVRT
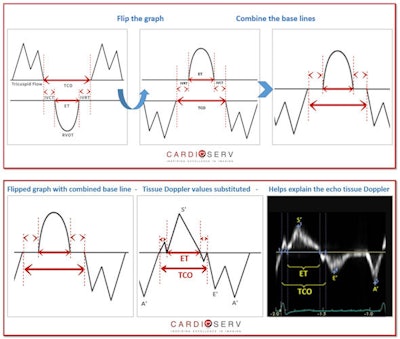
If you're having a hard time imagining how the tissue Doppler measurements relate to the original diagram, just flip the diagram upside down and place it next to your tissue Doppler image to better understand each time interval (see below).
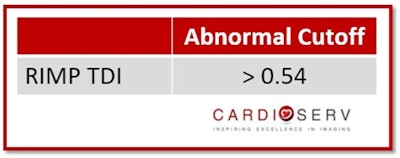
Reference ranges
If your machine is not set up with this measurement package, then the values will need to be calculated into the equation manually.
Limitations and advantages
The most obvious limitation of RIMP is obtaining a clear enough tissue Doppler reading to properly identify the nonejection periods of the heart. As I was looking through everyday examples of right heart tissue Doppler, it was hard to find images with clear enough waveforms to correctly identify the periods of IVRT/IVCT and therefore TCO. Other limitations include the following:
- RIMP varies with pressure and volume status
- Unreliable when RA pressure is elevated
- Shortens the IVRT
RIMP also has a number of important advantages:
- Reproducible
- Avoids geometric assumptions of complex RV geometry
- Allows for measurement of RIMP and S' wave from a single image
Here are some other RIMP tips for you:
- RIMP is another option to use for quantifying the RV function, and it can be obtained from the same frame as the S' wave measurement.
- While obtaining the S' wave, start looking to see if the TCO and ET times are noticeable.
- If the Doppler is not clear, pay special attention to the cursor placement through the annulus.
- Ensuring that the motion of the TV annulus moves toward the apex helps!
- Adjust gains to clean up the Doppler image.
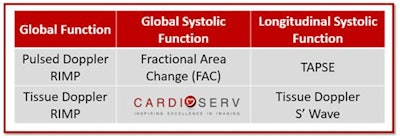
We have now covered four different methods that the ASE provides for quantifying RV function. Remember, the ASE recommends that we perform at least one or a combination of the following: TAPSE, S' wave, FAC, or RIMP. Please let us know how you are doing with implementing RV quantification into your labs!
References
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. American Society of Echocardiography website. http://asecho.org/wordpress/wp-content/uploads/2015/01/ChamberQuantification2015.pdf. Published 2015. Accessed March 1, 2017.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685-713.
Judith Buckland is president of CardioServ, a consulting firm focused on inspiring excellence in diagnostic imaging. Judith can be reached by email at [email protected] or via CardioServ's website.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.



















