
The right heart has jokingly been referred to as the organ's stepchild, with little attention paid to its size, function, and prognostic implications. To help with this often overlooked task, this article series reviews the proper methods to quantify the right heart for both size and function.
 Judith Buckland, president of CardioServ.
Judith Buckland, president of CardioServ.
We selected TAPSE and the S' wave as the initial function quantification methods to cover in our series due to their ease, reproducibility, and established prognostic value. However, TAPSE and the S' wave have limitations such as angle and load dependency. In addition, these techniques do not fully represent global RV function and are therefore susceptible to overestimation or underestimation.
FAC
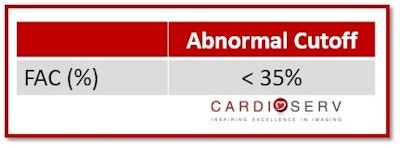
In this article, we'll discuss fractional area change (FAC), another method listed by the ASE for evaluating right ventricular function. A measurement that provides an estimate of the global RV systolic function, FAC is a formula for the percentage of area change within the RV between diastole and systole. A normal value for FAC is greater than 35%. Please do not confuse FAC with the ejection fraction (EF) percentage. Based upon the area change, the value will be less than the calculated EF percentage.
Although it provides a better estimate of global RV function, fractional area change -- as is the case with most quantitative methods -- has advantages as well as limitations. FAC has an established prognostic value and can serve as an independent predictor of heart failure, sudden death, stroke, and mortality in patients after pulmonary embolectomy. It also covers both the longitudinal and radial components of RV contraction and correlates well with cardiac MRI.
On the downside, FAC neglects the contribution of the right ventricular outflow tract (RVOT) to overall RV function. In addition, it suffers from limited interobserver reproducibility. However, FAC is still a great representation of the estimated global RV systolic function.
Performing FAC correctly
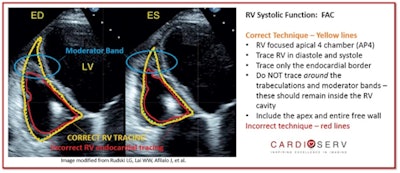
This method should be performed on the RV-focused apical 4 (AP4) view, which we described in part 1 of our series. Ensure that the entire RV is contained in the imaging sector during both systole and diastole. Then trace the RV area in diastole and systole (cm2), and be sure to include the trabeculae and apex within the cavity.
It's important to be aware of several pitfalls when measuring FAC:
- Avoid foreshortening of the RV.
- Be sure to include the entire apex and free wall.
- Trace the endocardial border (see the yellow line in the image below for an example of correct tracing).
- Do not trace the borders of the moderator band and trabeculae; only trace the RV endocardial border.
- Don't measure what you don't see! Remember, there are other methods (TAPSE or S' wave) you can use for evaluating RV function.
 All images courtesy of CardioServ.
All images courtesy of CardioServ.FAC reference values
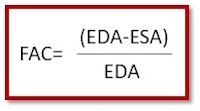
Fractional area change can be calculated by subtracting the end systolic area (ESA) from the end diastolic area (EDA) of the RV and then dividing that result by the EDA. This is a quick and easy calculation, so don't be afraid to use a calculator if your machine does not have a measurement package.
Normal FAC values are greater than 35%; anything less than that is abnormal.
In our next article, we'll review a fourth RV quantification method: the right ventricular index of myocardial performance (RIMP).
References
Guazzi M, Bandera F, Pelissero G, et al. Tricuspid annular pane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol. 2013;305(9):H1373-H1381. doi:10.1152/ajpheart.00157.2013.
Kossaify A. Echocardiographic assessment of the right ventricle, from the conventional approach to speckle training and three-dimensional imaging, and insights into the "right way" to explore the forgotten chamber. Clin Med Insights Cardiol. 2015;9:65-75. doi:10.4137/CMC.S27462.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. American Society of Echocardiography website. http://asecho.org/wordpress/wp-content/uploads/2015/01/ChamberQuantification2015.pdf. Published 2015. Accessed March 1, 2017.
Judith Buckland is president of CardioServ, a consulting firm focused on inspiring excellence in diagnostic imaging. Judith can be reached by email at [email protected] or via CardioServ's website.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.



















