NEW YORK CITY - A new technique for imaging microbubble ultrasound contrast agents shows promise for identifying prostate cancer even in patients with a negative MRI, according to a presentation delivered at the American Institute of Ultrasound in Medicine (AIUM) meeting.
A team led by Dr. Ethan Halpern of Thomas Jefferson University found that the technique, subharmonic imaging (SHI), showed contrast enhancement in the prostate of every subject in the study. Focal areas of contrast enhancement corresponded to cancer sites in 18% of targeted biopsies -- including nine patients whose cancer was not identified by MRI.
"Our urologists have an increasing number of patients where the MRI-guided biopsy produces no positive results, despite the fact that the MRI itself suggested something suspicious," Halpern told session attendees. "So they've been sending these patients to us for a second biopsy using ultrasound."
Biopsy improvement?
Prostate cancer accounted for 19% of new cancers among U.S. men in 2017, Halpern said, and the traditional core biopsy method finds 70% of these. However, studies of contrast-enhanced ultrasound-targeted biopsy suggest the technique has improved the detection of larger-volume and higher-grade prostate cancers compared to core biopsy.
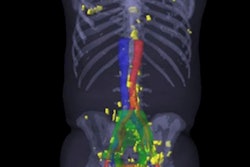
Subharmonic imaging visualizes microbubble ultrasound contrast agents with better signal suppression of background tissues than conventional contrast harmonic imaging. Halpern's group conducted a pilot study to evaluate the performance of contrast-enhanced subharmonic imaging for detecting prostate cancer.
"Contrast-enhanced subharmonic imaging has better suppression of background tissues compared to conventional contrast-enhanced ultrasound, improved signal-to-background ratio, and better resolution compared to color Doppler," Halpern said. "It also better localizes hyperemia."
The study included 55 patients referred for prostate biopsy who were imaged with a transrectal IC5-9D transducer on a modified scanner (Logiq E9, GE Healthcare) altered to perform subharmonic imaging. The patients received intravenous ultrasound contrast over 10 minutes. Their mean prostate-specific antigen (PSA) level was 8.6 ng/dL and mean glandular volume was 57 mL.
Images were acquired via conventional contrast harmonic imaging as well as subharmonic imaging, and they were evaluated using microbubble destruction pulses followed by maximum intensity projection (MIP) in combination with both imaging modes. The patients underwent prostate biopsy with up to six targeted cores with contrast-enhanced subharmonic imaging, followed by a 12-core systematic biopsy.
Halpern's group observed contrast enhancement with both conventional contrast harmonic imaging and subharmonic imaging, but subharmonic imaging provided improved contrast signal and tissue signal suppression relative to conventional harmonic imaging, he said. The researchers discovered that areas of increased vascularity were best identified with MIP subharmonic imaging, which also visualized microvascular architecture.
Subharmonic imaging identified prostate cancer in 24 of 55 patients, including nine of 31 patients with a negative prior prostate MRI, Halpern said. Among the nine patients with prostate cancer and negative prior MRI studies, six had a Gleason score of 6, two had a Gleason score of 7, and one had a Gleason score of 9.
Contrast-enhanced imaging showed one to three areas of increased enhancement per patient, and these areas were then targeted for biopsy. Among 660 systematic biopsy cores, 55 were positive (8.3%) for cancer. Among 247 targeted biopsy cores, 26 were positive (10.5%) for cancer.
The results led Halpern to conclude that subharmonic imaging is an effective tool for identifying prostate cancer.
"SHI is an independent predictor of the presence of prostate cancer, beyond baseline grayscale and Doppler imaging," he said. "And it's encouraging that additional cases of prostate cancer were found among patients with prior negative prostate MRI exams."