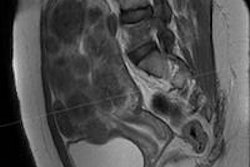
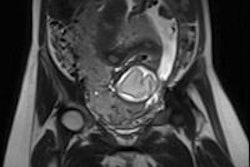
Cesarean delivery can change the angle of a woman's uterus from an anteflexed one, in which the fundus faces the abdominal wall, to a retroflexed one, in which it faces the sacrum, according to a study in the May issue of the Journal of Ultrasound in Medicine.
Because a retroflexed uterus can increase a woman's risk of uterine perforation during gynecologic surgery or the placement of an intrauterine device (IUD), the angle of her uterus after cesarean must be determined via ultrasound, wrote a team led by Dr. Andrea Agten of St. George's University Hospitals in London.
"Over the years, reports have associated a retroflexed uterine position with an increased surgical complication rate (e.g., uterine perforation) ... [and] although in many cases perforations are innocuous, some lead to infections, hemorrhage, and trauma to other abdominal organs," Agten and colleagues noted. "Therefore, all women with a history of cesarean delivery should undergo a transvaginal ultrasound examination before any gynecologic surgery or IUD placement" (J Ultrasound Med, May 2018, Vol. 37:5, pp. 1179-1183).
Which angle?
One of the ways the position of the uterus is assessed is by its flexion angle, which is the measure between the uterus and the cervix. Gauging uterine position is crucial for successful gynecologic procedures such as dilation and curettage, endometrial biopsy, and IUD insertion, the team wrote.
 Dr. Andrea Agten of St. George's University Hospitals.
Dr. Andrea Agten of St. George's University Hospitals.The researchers conducted the study because they had observed an increase in retroflexed uteri in their practice. And because the number of cesarean deliveries has also increased, they sought to investigate whether this higher incidence of retroflexed uterus could be caused by cesarean delivery.
The study included data from 173 patients who had undergone transvaginal ultrasound before and after either vaginal or cesarean delivery between 2012 and 2015, excluding women who had undergone a previous cesarean delivery. Two radiologist readers measured flexion angles from these exams before and after the women gave birth, and they compared them between women with vaginal and cesarean deliveries.
Of the 173 women, 107 had vaginal deliveries (62%) and 66 had cesareans (38%). The mean interval between scans was 18 months; interreader agreement for flexion angles was almost perfect, the researchers found (0.939 before delivery and 0.969 after, p < 0.001).
There was no significant difference in mean flexion angles between the uterus and the cervix for either type of delivery on antepartum ultrasound (145.8° for vaginal delivery and 154.8° for cesarean). But mean postpartum flexion angles increased significantly after cesarean, at 152.8° for women who had a vaginal delivery compared with 180.4° for those who underwent a cesarean (p < 0.001).
The change in flexion angle translated into a shift from anteflexed to retroflexed in more of the women who underwent cesarean delivery than those who had a vaginal delivery (29% versus 13%, p = 0.003).
"Our study showed that cesarean delivery can change the natural position of the uterus ... [and that it was] associated with the new development of a retroflexed uterus in one-third of our patients," Agten's group wrote.
Avoiding complications
Because a retroflexed uterine position has been associated with surgical complications, it's important for a woman's health going forward to assess the position of her uterus after she has had a cesarean, Agten and colleagues wrote.
"Cesarean delivery can change the uterine flexion angle to a more retroflexed position," the researchers concluded. "Therefore, all women with a history of cesarean delivery should undergo a transvaginal sonography examination before any gynecologic surgery or IUD placement to reduce the possibility of surgical complications."