A woman's body fat index (BFI) measured by ultrasound appears to be a better gauge of the possibility of obstetric complications than body mass index (BMI), according to research presented at the recent American Institute of Ultrasound in Medicine (AIUM) meeting in New York City.
Presenter Dr. Ahmed Nassr, PhD, of Baylor College of Medicine hypothesized that measuring a woman's body fat index at the same time that a fetal anatomic survey is conducted could offer more information than BMI data regarding her risk of pregnancy complications. The index specifically measures central fat, he told session attendees.
"Our objective was to evaluate BFI as a risk factor for obstetric complications predisposed by maternal overweight, and to compare the predictive performance of BFI to conventional BMI for these complications," Nassr said.
A new measure
The study was conducted between 2014 and 2015 and included 389 nondiabetic pregnant women referred to Baylor for fetal anatomic surveys between 18 and 24 weeks of gestation. The women's mean age was 29 years.
Study participants underwent visceral and subcutaneous fat measurements at the time of the fetal anatomic survey. The group calculated BFI as subcutaneous fat measurement multiplied by visceral fat measurement (in mm), then divided by height (in cm). For the women included in the study, median BMI was 25 and BFI was 0.78.
Nassr's team then followed the women through their pregnancies, noting any complications such as gestational diabetes or hypertensive disorders and the mode of delivery, as well as any delivery-related events. The group evaluated BMI and BFI separately for each obstetric complication.
The researchers found that a BFI of more than 0.5 was associated with a higher risk of developing gestational diabetes than a BMI of more than 25. In addition, a BFI of more than 0.8 was associated with a greater risk of developing hypertensive disorders of pregnancy and needing a cesarean section than a BMI of more than 25.
"Body fat index is a novel ultrasound measure that can be taken at the time of fetal anatomic survey with no additional burden," Nassr said. "It specifically recognizes central fat and seems to be more informative than BMI in terms of prediction of obstetric complications."
Obesity's effect
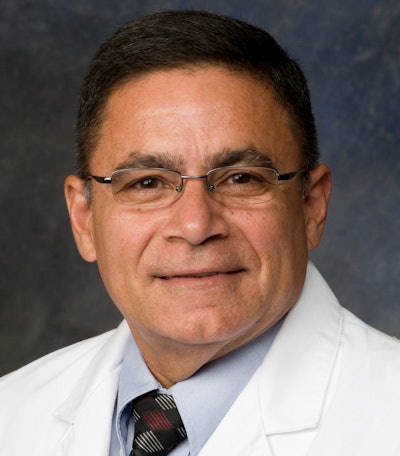 Dr. Manuel Rivera-Alsina from Methodist Health System Dallas.
Dr. Manuel Rivera-Alsina from Methodist Health System Dallas.In a related study delivered in the same session, Dr. Manuel Rivera-Alsina of Methodist Health System Dallas discussed the effect of maternal obesity on the visualization of fetal anatomy.
The research included 529 patients with singleton pregnancies between 17 and 23 weeks of gestation between March 2015 and June 2017. Of the 529 patients, 316 were obese (59.7%) and 213 (40.2%) were not.
Rivera-Alsina and colleagues classified the women defined as obese into three categories:
- Category 1 (BMI = 30-34): 105 women (33.2%)
- Category 2 (BMI = 35-39): 153 women (48.4%)
- Category 3 (BMI ≥ 40): 58 women (18.4%)
| Complications by BMI category | |||
| Nonobese | Category 1 | Category 2 | Category 3 |
|
|
|
|
| 6 total | 7 total | 13 total | 11 total |
The odds of suboptimal visualization at first ultrasound in obese women were 43 times higher than in nonobese women, the researchers found. In addition, for obese women compared with those who were not obese, the odds of having fetal anomalies were four times higher (p = 0.002) and the odds of undergoing fetal echocardiography were 24 times higher (p = 0.001).
Rivera-Alsina and colleagues found that fetal echo was needed in 60% of women with a BMI of 35 to 39 and 87.2% of women with a BMI of at least 40.
The study results have prompted Rivera-Alsina's department to change how patients are counseled about their expectations for initial ultrasound exam outcomes, as well as to consider fetal echocardiography for women who fall into categories 2 and 3, he said.
"We let women know that there may be visualization problems at their first fetal ultrasound, and to go to fetal echo right away if we don't see heart structures on the initial ultrasound scan," he said.