When lower extremity duplex ultrasound screening (LEDUS) protocols for the trauma department are refined, overuse of hospital resources is reduced by more than a third -- and without negative effect on patient outcomes, according to a new study published June 5 in the Journal of Surgical Research.
The findings translate to more efficient trauma departments -- and better patient care, wrote a team led by Dr. Jennifer Baker of the University of Cincinnati in Ohio.
"Refinement of LEDUS protocols can decrease overutilization of hospital resources without compromising trauma patient outcomes," the researchers concluded.
A tool called the risk assessment profile (RAP) is typically used in the trauma center to identify patients who would most benefit from lower extremity duplex ultrasound screening. But it can lead to overuse of imaging and needs refinement, Baker's group wrote.
The researchers conducted a study for which they hypothesized that revising their hospital's LEDUS protocol so that screening ultrasound examinations were performed in patients with a RAP score ≥ 8 within 48 hours of admission would reduce the number of screenings performed -- without changing patient outcomes.
The study included 1,014 trauma patients admitted from July 2014 to June 2015 and July 2016 to June 2017. From 2014 to 2015, patients with a RAP score ≥ 5 had weekly LEDUS examinations starting on the fourth hospital day, while from 2016 to 2017, the protocol changed to screening patients with a RAP score ≥ 8 by the second hospital day. Both protocols included screening with weekly ultrasound after the first examination. Baker's team gathered data on demographics, injury characteristics, LEDUS exam findings, and venous thromboembolism incidences.
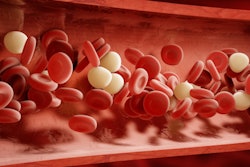
The group found that from 2014 to 2015, 602 patients underwent LEDUS exams, but from 2016 to 2017, only 412 patients did: a 32% drop. Significantly, the team noted no difference in the number of patients diagnosed with deep vein thrombosis (DVT) or pulmonary embolism between the two protocols; in fact, DVT was often identified in the first LEDUS exam in both year groups.
Regarding those patients who received a DVT diagnosis on first LEDUS exam, the group also found the following:
- These patients had significantly higher RAP scores than those who did not have a DVT diagnosis (12 versus 10).
- The time to their first LEDUS exam was shorter (one day versus three days).
- The DVT diagnosis was made more quickly (two versus four days).
A simple change to protocol can make a big difference without harming patients, according to the researchers.
"[This protocol change caused] no significant difference ... in the number of patients diagnosed with DVT or pulmonary embolism," they concluded.