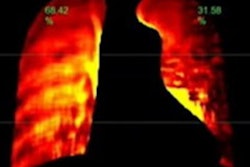
The use of ventilation/perfusion (V/Q) SPECT scans to rule out pulmonary embolism (PE) is evolving. What used to be the definitive test for PE is shifting into a role that harmonizes with the use of pulmonary CT angiography (CTA), according to an article in the American Journal of Roentgenology.
The authors looked at evidence, practice, problems, and research needs for PE diagnosis, while recommending diagnostic approaches for different patient groups. For example, while the use of V/Q in conjunction with SPECT/CT has improved clot detection sensitivity compared with planar imaging, CT's additional radiation dose is a concern, wrote Dr. Darlene Metter from the University of Texas Health Science Center at San Antonio, along with colleagues from two other U.S. institutions.
"Although advances in tomographic imaging have certainly improved the sensitivity of V/Q scans for the diagnosis of PE, they may lead to overdiagnosis by revealing small and clinically insignificant PEs," and overtreatment of these clinically insignificant embolisms is also a problem, the authors wrote (AJR, March 2017, Vol. 208:3, pp. 489-494).
Scanning options
Three lung perfusion acquisition techniques can be used after the administration of albumin radioisotopes labeled with technetium-99m (Tc-99m): planar imaging, SPECT, and SPECT/CT, they wrote. Contrast resolution is lowest with planar imaging, higher with SPECT, and highest with SPECT/CT, which provides CT-based attenuation correction and anatomic correlation. SPECT/CT increases the specificity of the scan by delineating lobar and segmental anatomy and underlying lung disease.
The choice of technique depends on user preference for perfusion defect resolution and correlative ventilation with anatomic detail, Metter and colleagues wrote.
Planar imaging should include the entire lung, optimally with eight static views, each 45° apart. Ventilation imaging is usually performed along with lung perfusion to characterize perfusion defects as matched, mismatched, or a combination called reverse mismatched, when a ventilation defect is more abnormal than a perfusion defect.
Ventilation radiopharmaceuticals include gases, aerosolized liquid droplets, and aerosolized solid particles. In the U.S., 58% of ventilation studies are performed using aerosolized liquid droplets that contain one of the Tc-99m-labeled radiopharmaceuticals, they wrote.
Reporting for V/Q scans using the probabilistic system -- based on the probability that a suspicious area is a clot -- has raised concerns about the outcomes of scans indicating a low probability of PE, and since 1995, steps have been taken to move away from this kind of reporting.
Analysis of data from the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED) II trial showed a PE incidence of 6.7%, raising the question of what the ultimate clinical outcome would be for these patients. A 2016 analysis determined that the incidence of nonfatal PE was 0.13%, with fatal PE at 0%. The recommended "no evidence of PE" designation for the low-probability scan is now incorporated into the trinary V/Q scan interpretation system, the authors wrote.
With the rise of CT angiography scans, investigators in 2008 proposed the Modified PIOPED II V/Q reporting criteria, similar to CTA reporting criteria. Results were designated "PE present" or "PE absent," eliminating use of the probabilistic scale. Low and intermediate probabilities were designated nondiagnostic.
"The two major benefits of perfusion-only imaging are the lower radiation dose and lower cost," Metter and colleagues wrote. "Pulmonary CTA delivers a much higher radiation dose to patients and, especially, to the female breast, which is particularly radiosensitive in young women.
The data are relevant because 60% of PE scans are performed on women, more than one-quarter of whom are younger than age 40, and the whole-body effective dose of pulmonary CTA is about five times that of the V/Q scan at less than 1.5 mSv. Radiation dose can be further reduced using perfusion-only imaging, which is recommended for PE evaluation of pregnant patients.
The 'trinary system'
To replace the binary either/or probabilistic system of PE reporting, researchers from Montefiore Medical Center in New York City created the trinary system, which classifies embolisms as positive, negative, or indeterminate.
High-probability scans are placed in the PE-positive category, while negative studies include scans with normal, very low, or low probabilities of PE. Nondiagnostic scans indicate an intermediate or indeterminate result.
Stein at al showed that a well-defined segmental mismatch can be designated PE-positive with a positive predictive value of 86% -- 100% if the patient also had a high pretest likelihood of PE, the group noted.
Normal V/Q SPECT scans can exclude PE with a high negative predictive value, but the increased contrast resolution of SPECT and the anatomy displayed by hybrid studies like SPECT/CT show even greater sensitivity and specificity. However, limitations in existing studies mean that a multicenter prospective trial with consecutive patients, blinded interpretations, and an independent reference standard, or independent composite reference standard, are needed to definitively compare the accuracy of V/Q SPECT with that of V/Q planar imaging and pulmonary CTA, Metter and colleagues wrote.
In 2009, the European Association of Nuclear Medicine (EANM) recommended V/Q SPECT over V/Q planar imaging, and the EANM considers the probabilistic reporting system to be obsolete, recommending positive or negative designations similar to the trinary system, the authors wrote.
Overdiagnosis and overtreatment
Strong evidence indicates that healthy individuals pass small PEs, so detecting very small clots is probably not valuable. Small clots don't need to be treated unless there are associated complications such as deep vein thrombosis (DVT). The American College of Chest Physicians recommends surveillance over anticoagulation for patients with a low risk of recurrent venous thromboembolism, and anticoagulation over surveillance for high-risk patients.
"Unfortunately, in the United States, the practice of defensive medicine means that all PEs, regardless of size, most often will be treated," the authors wrote. "This is not the case in most countries outside of the United States. It is hoped that support from credible sources, such as the American College of Chest Physicians, will help change this policy of overtreatment."
There is an ongoing multicountry prospective study (NCT 01455818) in which treatment is being withheld in patients with small PEs, offering more support for not using anticoagulants in these patients, the team wrote.
"Pulmonary CTA clearly detects more PEs than does V/Q planar imaging," they wrote. "Despite this observation, three-month follow-up of initially negative pulmonary CTA and V/Q scans are essentially identical, further confirming the clinical usefulness of a negative V/Q scan."
Recommendations for diagnosis
If there is concern about PE, a chest radiograph should be obtained first, the group wrote. If the findings are normal or near normal, or if there is edema, a V/Q scan is indicated. If chest radiography is significantly abnormal, and if the patient is clinically unstable, pulmonary CTA should be performed absent contraindications such as renal insufficiency. If the CTA or V/Q results are discordant with Doppler ultrasound or clinical assessment, the other imaging modality should be used to resolve the discrepancies.
In pregnant patients suspected of having a PE, Doppler ultrasound should be performed first, with treatment indicated if results are positive. If ultrasound is negative, then a chest radiograph should be obtained. If the radiograph is normal, a perfusion-only lung scan at reduced dosage is recommended. If chest radiography is significantly abnormal, pulmonary CTA is preferable, according to the authors.
CT and hybrid imaging have created the dilemma of overdiagnosis and overtreatment of insignificant PE. Considering the practice of defensive medicine in the U.S., "the use of V/Q planar imaging is favored over tomographic techniques at this time," they wrote.
"The recent American College of Chest Physicians policy statement supporting surveillance over treatment for small PEs and the current international prospective trial assessing the significance of the small PE may change practice recommendations in the United States regarding optimal V/Q imaging in favor of the tomographic technique," they added.