Biomarkers derived from contrast-enhanced ultrasound scans (CEUS) -- such as differences in the arrival time of contrast -- can help predict whether cirrhotic nodules will convert to liver cancer, according to a study published online October 23 in the American Journal of Roentgenology.
Approximately 80% of liver cancers develop in patients with chronic hepatitis or cirrhosis, wrote a team led by Dr. Manxia Lin of Sun Yat-Sen University in Guangzhou, China. In these patients, the cancer evolves over time: Regenerative nodules can progress to dysplastic nodules and, from there, develop into early liver cancer.
But since not all regenerative nodules and dysplastic nodules necessarily progress to cancer, the study findings address the long-standing problem of how to characterize and follow these nodules.
"Not all ... nonmalignant cirrhotic nodules progress to hepatocellular carcinoma," the group wrote. "Thus, it is important to identify the variables in predicting malignant transformation to better customize appropriate follow-up algorithms on the basis of risk."
The researchers' goal was to "establish the predictive significance of initial noninvasive clinical and sonographic variables associated with nodules that eventually transformed into hepatocellular carcinoma versus those that did not and to identify sonographic changes during follow-up that indicated malignant transformation," the authors wrote. The study included 39 patients with 44 confirmed cirrhotic nodules who underwent CEUS and then follow-up conventional ultrasound every three to four months afterward.
The team found that 31.8% of the nodules became cancerous after a median follow-up time of 26.7 months. And these nodules had a particular sonographic marker: The difference in contrast arrival time between the cirrhotic nodule and the liver on CEUS helped predict eventual cancer conversion risk.
"At initial detection, nodule size and a contrast arrival time difference between the nodule and liver of more than 0.5 second were independent predictors for malignant transformation," Lin's team noted.
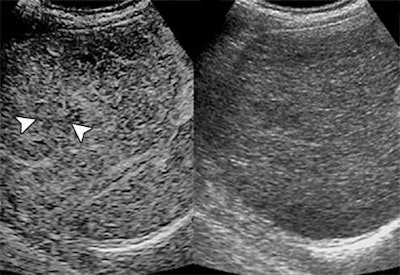 Shown are two ultrasound images of a 69-year-old man with cirrhotic nodule, one contrast-enhanced (left) and one conventional (right). At initial detection, contrast arrival time difference between nodule and liver was 1.87 seconds. At 30.07 seconds, nodule (arrowheads, left image) is isoenhanced compared with surrounding liver. Images courtesy of ARRS.
Shown are two ultrasound images of a 69-year-old man with cirrhotic nodule, one contrast-enhanced (left) and one conventional (right). At initial detection, contrast arrival time difference between nodule and liver was 1.87 seconds. At 30.07 seconds, nodule (arrowheads, left image) is isoenhanced compared with surrounding liver. Images courtesy of ARRS.The researchers also found that an absolute growth rate of cirrhotic nodules of 5 mm or greater in six months or a relative growth rate of 30% or greater in six months could predict a nodule's conversion to cancer with a specificity of 100% and a positive predictive value of 100%. Conversely, a lack of echogenicity change and threshold growth was highly accurate in excluding conversion to cancer (sensitivity of 100% and negative predictive value of 100%).
These CEUS biomarkers could make the Liver Imaging Reporting and Data System (LI-RADS) system more precise, Lin and colleagues concluded.
"These additional imaging features may have the potential to be adopted as ancillary or even major features to stratify probability for hepatocellular carcinoma in the CEUS LI-RADS system," they wrote.