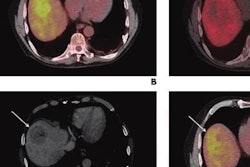
Patients with a common form of liver cancer experienced better treatment outcomes in a recent study when clinicians paired transarterial radioembolization (TARE) with microbubble destruction by ultrasound (US) waves, according to early results published on December 15 in Radiology.
The study is believed to be the first in-human clinical trial evaluating the use of microbubble destruction and TARE to treat hepatocellular carcinoma (HCC). Based on the early findings, the combination looks like a promising method to improve TARE outcomes.
"Early results indicate that US-triggered [microbubble] destruction sensitizes tumors to radioembolization and may improve both tumoral response and overall participant survival," wrote the authors, led by John Eisenbrey, PhD, an associate professor of radiology at Thomas Jefferson University in Philadelphia, PA.
While TARE treatment is not curative, the radioembolization therapy is growing in popularity for some patients with HCC. At Thomas Jefferson University, clinicians often use TARE to downstage tumors in patients who are unable to meet the criteria for liver transplant or bridge to transplant.
Despite its increasing popularity, TARE is not as effective as clinicians would like. Preclinical research in rodents suggests that using external ultrasound waves to destroy microbubble contrast agents may improve TARE response. The idea is that the energy of the destroyed contrast agents damages the tumor blood vessels, making them more sensitive to the effects of radiation.
For the study, eligible participants were randomly assigned to receive TARE alone or TARE in combination with ultrasound-triggered microbubble destruction. Patients in the latter group underwent three different ultrasound sessions -- one just hours after TARE treatment, a second about a week after TARE, and a third about two weeks after TARE.
The new, preliminary results show that the preclinical research may translate to humans with HCC. In the 28-person study, a significantly greater proportion of patients achieved partial or complete liver tumor response if they received both TARE and ultrasound-triggered microbubble destruction.
In addition, more patients in the combined treatment group qualified for orthotopic liver transplant. Of the eligible patients, 70% in the TARE and ultrasound-triggered microbubble destruction group and 50% in the TARE only group were listed to undergo liver transplant.
| Impact of ultrasound microbubble destruction on treatment outcomes for HCC patients | ||
| TARE alone
(n = 10) |
TARE + ultrasound-triggered microbubble destruction
(n = 15) |
|
| Partial or complete tumor response | 50% | 93% |
| Required retreatment | 55% | 35% |
| Qualified for liver transplant | 40% | 67% |
| Listed for liver transplant | 20% | 47% |
The safety results also looked good for the group that underwent TARE with ultrasound-triggered microbubble destruction. The group that received both techniques experienced no significant differences in liver function tests, temperature, heart rate, and blood pressure.
As for mortality rates, one patient in the combination group died from hip fracture complications, while three patients in the TARE group died from cancer progression. In addition, fewer patients who underwent TARE with ultrasound-triggered microbubble destruction required tumor retreatment.
While the difference in mortality and retreatment rates did not reach statistical significance, the preliminary results still make the combination treatment look promising given the study's small sample size. The authors are continuing the trial with the goal to reach a final sample size of more than 100 participants.
"Our findings are really setting the stage for a whole range of studies to be done in humans," stated Eisenbrey in a press release. "This approach could be effective in treating metastatic liver tumors, but also other types of primary cancer. The bubbles themselves can also be engineered to deliver chemotherapy or oxygen as they burst. This is really the tip of the iceberg."