With help from artificial intelligence (AI) technology, novice users can acquire high-quality bedside cardiac point-of-care ultrasound (POCUS) exams in the COVID-19 intensive care unit (ICU), according to a recent article in JACC: Case Reports.
In an open access case report, researchers from Northwestern University Feinberg School of Medicine in Chicago shared a case series of five patients who had received AI-guided cardiac POCUS exams acquired by critical care physicians without any formal training in ultrasound. The POCUS exams affected decision-making and patient care in all five cases.
"Our discussion showcases the use of AI in medicine, which can simplify tasks that traditionally required highly trained individuals to complete," wrote Dr. Baljash Cheema and colleagues. "As our knowledge of AI algorithms increases, we will undoubtedly see more and more of their use in clinical practice."
The institution deployed Caption Guidance, an AI-based software application developed by Caption Health to guide novice users in acquiring cardiac ultrasound exams. The software provides real-time prescriptive guidance to steer the user's transducer position and hand movements to acquire the desired cardiac ultrasound image, according to the authors. It also displays the current image quality and, when appropriate, automatically captures the image, they said.
In addition, Caption Guidance can automatically -- independent of chamber volumes -- detect ejection fraction with similar accuracy to that of the standard volume-dependent approach, according to the researchers. After acquisition, the images are uploaded to the institution's PACS for overreading by the attending cardiologist.
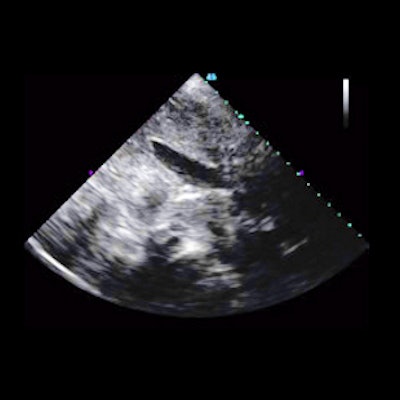
In one case, the AI-guided cardiac ultrasound exam showed a severe dilated and dysfunctional right ventricle, a hyperdynamic left ventricle, a mitral valve prosthesis, and a dilated inferior vena cava in a 65-year-old woman with a history of rheumatic heart disease and suspicion of COVID-19.
As a result, the patient's primary insult was determined to be progressive pulmonary hypertension with subsequent right ventricular failure. The patient, who remained negative for SARS-CoV-2, improved with heart failure management, according to the authors.
In another case, a 76-year-old woman with acute hypoxemic respiratory failure from acute left ventricular failure received a POCUS exam that demonstrated new severe left ventricular dysfunction.
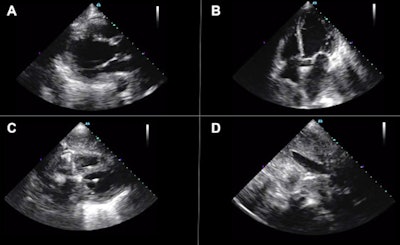 Bedside artificial intelligence-guided cardiac ultrasound revealed new severe left ventricular dysfunction (automated ejection fraction estimated to be 27%) and normal right ventricular function with a noncollapsible inferior vena cava. (A) Parasternal long-axis, (B) apical four-chamber, (C) subcostal four-chamber, and (D) subcostal inferior vena cava views are provided. Image courtesy of JACC Case Reports and Dr. Baljash Cheema, et al. Licensed under CC BY-SA 4.0.
Bedside artificial intelligence-guided cardiac ultrasound revealed new severe left ventricular dysfunction (automated ejection fraction estimated to be 27%) and normal right ventricular function with a noncollapsible inferior vena cava. (A) Parasternal long-axis, (B) apical four-chamber, (C) subcostal four-chamber, and (D) subcostal inferior vena cava views are provided. Image courtesy of JACC Case Reports and Dr. Baljash Cheema, et al. Licensed under CC BY-SA 4.0.Her SARS-CoV-2 test was negative, and the treating clinician changed the treatment strategy to a regimen for acute heart failure. The patient's condition worsened, however, and she died after a transition to comfort-focused care, according to the researchers.
"Reviewing these cases may suggest how this technology could be expanded to additional units within the hospital utilizing POCUS, including the emergency department, hospital wards, and perioperative medicine, and potentially limit sonographer exposure to patients with COVID-19," the authors wrote. "This technology may also have a role outside the walls of the hospital, particularly in resource-limited settings where cardiac sonographers are not readily available."
In an accompanying editorial comment, Dr. Sameer Raina and Dr. Partho Sengupta of West Virginia University School of Medicine in Morgantown, WV, noted that AI-based POCUS -- in its current form -- is "at best a primitive avatar of a navigation system that helps create a basic set of information to be interpreted by an expert health care professional."
"The current pandemic, however, has come as a shot in the arm and has set an excellent tailwind for a bright future for this technology," the authors concluded.