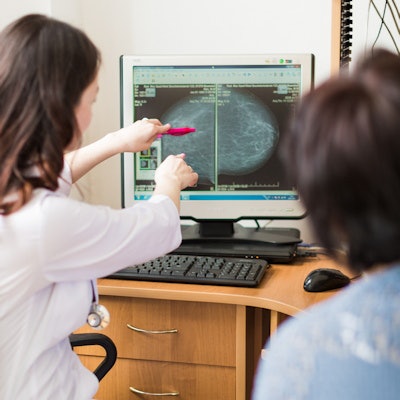
Now is not the time to close the door on screening breast ultrasound trials, despite the findings of a research study published earlier this year, according to an opinion piece by Dr. Paula Gordon and Dr. Wendie Berg, PhD, published August 17 in Radiology.
In their new opinion piece, Gordon of the University of British Columbia and Berg from the University of Pittsburgh responded to the findings of a study published in Radiology on January 12 by first author Dr. Ann Yi of Seoul National University Hospital Healthcare and colleagues. In that study, the researchers examined the use of ultrasound as a supplemental screening modality for average-risk women who underwent digital mammography and/or digital breast tomosynthesis (DBT).
Yi et al found that supplemental ultrasound screening made a "modest" contribution, detecting 3.2 extra cancers missed by mammography in 1,000 women with dense breast tissue. But no additional cancers were detected in women with nondense breasts, and the group that received ultrasound had a higher abnormal interpretation rate and lower specificity.
In an invited commentary piece published along with Yi et al, Dr. Habib Rahbar from the University of Washington suggested that the findings show it is time to "close the chapter" on screening breast ultrasound. He suggested that MRI and contrast-enhanced mammography-based approaches to screening are superior to ultrasound for improving cancer detection rates.
"[It] is likely time to close the chapter on [ultrasound] screening trials," Rahbar posited.
But Gordon and Berg believe that ultrasound still has a role to play in breast screening.
"Ultrasound, with all its limitations, remains an important option for supplemental screening in women with dense breasts and does not require injection of an intravenous contrast agent," they wrote.
Gordon and Berg said the results of Yi et al are similar to previous studies of screening ultrasound, where the incremental cancer detection rate averaged 2 to 2.7 and added recalls averaged 7.5% across more than 425,000 screenings.
"These results reflect findings seen only at ultrasound, excluding the cancers seen also at mammography, and therefore biasing against ultrasound," they wrote.
Gordon and Berg said both ultrasound and MRI reduce interval cancer rates and that the incremental cancer detection rate of MRI averages 10 of 1,000 after DBT with added recalls averaging 21.5% in women at average risk.
They also said there is insufficient MRI capacity for women with dense breasts who are at greater-than-average risk.
"Contrast-enhanced mammography is not yet widely available but may be a good alternative to MRI in women with dense breasts," they wrote.
Gordon and Berg said women should be informed of the possibility of a false alarm and that recalls decrease with incidence screening.
"The minimal discomfort of ultrasound-guided biopsy, when indicated, is a small price to pay for the benefit of early detection of invasive malignancy," the authors wrote.
Rahbar responded to the opinion piece, clarifying that while Yi et al showed unsatisfactory results with the addition of screening ultrasound, ultrasound still has value.
"Screening ultrasound should be continued for patients who will truly benefit from it, and we should make more efforts to find evidence that supports the provision of more individualized screening options for women," he wrote.