Increased liver stiffness found on shear wave elastography (SWE) is tied to cardiovascular problems on follow-up in patients with Fontan circulation, a study published August 2 in the American Journal of Roentgenology found.
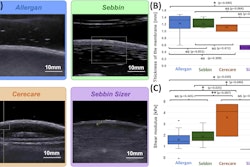
Researchers led by Betul Derinkuyu, MD, from Cincinnati Children's Hospital Medical Center found that in these patients, increased initial liver stiffness was associated with portal hypertension and circulatory failure during follow-up. However, this approach had just moderate performance in predicting outcomes.
"Ultrasound SWE may play a role in post-Fontan surveillance, supporting tailored medical and surgical care," Derinkuyu and co-authors wrote.
The Fontan circulation consists of low cardiac output and elevated central venous pressure, though with the absence of a subpulmonary ventricle. Fontan operations make symptoms less severe, but they may also cause liver congestion with associated progressive liver fibrosis.
SWE measures tissue stiffness by producing an acoustic radiofrequency force impulse. Derinkuyu and colleagues wanted to investigate potential links between liver stiffness measured using SWE in patients with Fontan operations and the occurrence of portal hypertension and Fontan circulatory failure during follow-up.
The researchers included retrospective data from 119 individuals with a median age of 19.1 years. All patients included in the study were at least 10 years old. Also, of the total, 61 individuals were female and 58 were male. The study population consisted of individuals with Fontan circulation who underwent liver ultrasound with 2D SWE from 2015 to 2022 and one year or more of clinical follow-up.
The team used varices, ascites, splenomegaly, and thrombocytopenia (VAST) scores, which range from 0 to 4, as a marker of portal hypertension on initial ultrasound and one-year follow-up imaging using ultrasound, CT, or MRI.
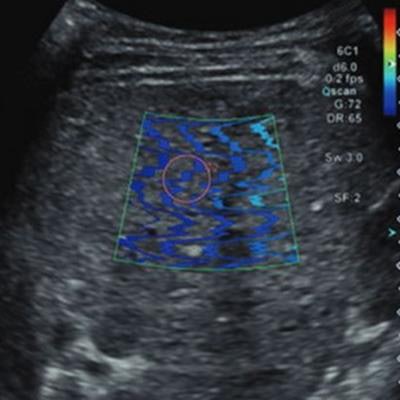
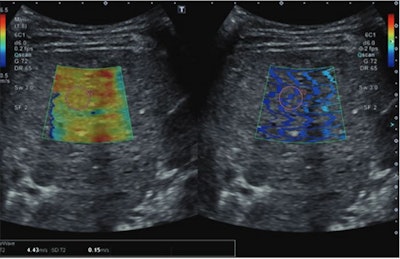 Ultrasonic images show a 15-year-old patient with prior Fontan circulation and high initial liver stiffness (4.43 m/s). The patient subsequently developed Fontan circulatory failure during follow-up at age 19 and underwent heart transplantation. The left image is a color elastogram (scale to left), and the right image is wave propagation image, reflecting quality of shear-wave acquisition. The pink circle indicates the sample region of interest. Image courtesy of the ARRS.
Ultrasonic images show a 15-year-old patient with prior Fontan circulation and high initial liver stiffness (4.43 m/s). The patient subsequently developed Fontan circulatory failure during follow-up at age 19 and underwent heart transplantation. The left image is a color elastogram (scale to left), and the right image is wave propagation image, reflecting quality of shear-wave acquisition. The pink circle indicates the sample region of interest. Image courtesy of the ARRS.The researchers found that the median initial liver stiffness was 2.22 m/s, the median initial VAST score was 0, and the median follow-up VAST score was 1 (p = 0.04). Also, Fontan circulatory failure occurred in 37 patients (31%), with a median follow-up of 3.4 years.
The team also reported that initial liver stiffness was higher in patients with follow-up VAST scores of 1 or higher (2.37 m/s) than follow-up VAST scores of 0 (2.08 m/s, p = 0.005). Stiffness was also higher in patients with Fontan circulatory failure (2.43 m/s) than those without (2.1 m/s) such failure at follow-up (p < 0.001).
The researchers also found that initial liver stiffness was the only significant independent predictor of Fontan circulatory failure, with an odds ratio of 3.76 (p < 0.001). Initial liver stiffness also had an area under the curve (AUC) of 0.7 for predicting a VAST score of one or greater, which included a sensitivity of 79% and a specificity of 57%. This was at a threshold of greater than 2.11 m/s. Initial liver stiffness also had an AUC of 0.74 for predicting Fontan circulatory failure with a threshold of 2.12 m/s. This included a sensitivity of 84% and specificity of 52%.
While the study authors called for more research to confirm their results, including prospective and longitudinal studies, they suggested that liver stiffness measurements via SWE could help predict future adverse events in these patients. Surveillance imaging in this setting could support tailored medical and surgical care.
"Such prediction may allow individualized timely interventions, thereby potentially decreasing Fontan-related morbidity and mortality," the authors wrote.
The study can be found in its entirety here.