Elastography could help with treatment strategies for colorectal cancer patients, a study presented November 26 at the RSNA annual meeting found.
In his presentation, Jae Seok Bae, MD, from Seoul National University Hospital in South Korea presented research that found that shear-wave velocity values measured after chemotherapy showed predictive performance in chemotherapy responsiveness in patients with colorectal cancer liver metastases.
 Jae Seok Bae, MD, from Seoul National University Hospital presented research at RSNA showing the efficacy of shear-wave elastography in predicting chemotherapy response in colorectal patients.Amerigo Allegretto
Jae Seok Bae, MD, from Seoul National University Hospital presented research at RSNA showing the efficacy of shear-wave elastography in predicting chemotherapy response in colorectal patients.Amerigo Allegretto
“I hope that this [elastography] will be helpful in predicting the overall [treatment] response,” Bae said.
Chemotherapy is the standard treatment for treating colorectal cancer with liver metastases. Assessing treatment response is important for determining the chemotherapy regimen, such as adjusting which chemotherapeutic agents are used. Early changes in the regiment often lead to prognosis.
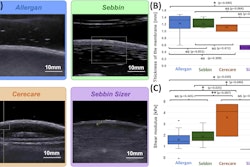
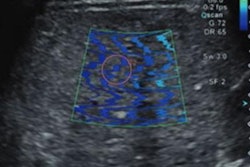
Shear-wave elastography measures changes in tumor stiffness between and after chemotherapy to predict pathological response in patients. Previous studies have shown its efficacy in this area for breast cancer.
Bae and colleagues sought to study the prognostic role of shear-wave velocity value for predicting chemotherapeutic response and progression-free survival in colorectal cancer patients. In its prospective single-center study, the team used shear-wave elastography on metastases before and after the start of chemotherapy.
The researchers categorized the chemotherapeutic response of study participants by either responders including complete remission and partial remission, and nonresponders including stable disease and progressive disease.
In total, the group included data collected between 2018 and 2021 for 67 patients. Of these, 34 were responders and 33 were nonresponders. It found that the receiver operator curve of elastography was high 0.84. This also included a sensitivity of 97% and a negative predictive value of 95.2%, respectively, with a cutoff value of a 13% decrease.
Additionally, the researchers found that the change in shear-wave velocity value was tied to progression-free survival, with a hazard ratio of 1.02. Finally, the shear-wave velocity value was also tied to being a nonresponder and the number of liver metastases (five or above). These included hazard ratios of 2.861 and 2.55, respectively. All achieved statistical significance.
Bae said that based on these results, shear-wave value shows a “meaningful” performance when predicting chemotherapeutic response. However, he added that no additional research is currently planned, saying that it’s challenging to recruit study participants.