Morphologic features of axillary nodes on sonography are reliable indicators in predicting metastasis, according to research published October 24 in Clinical Imaging.
A team led by Anubha Wadhwa, MD, from Froedtert Hospital in Milwaukee, WI, found that greater cortical thickness and the absence of a normal hilum had the highest positive predictive value (PPV) for metastatic disease.
“Using clinical history in conjunction with imaging findings will help improve the accuracy of axillary nodal biopsies, especially for incidental nodes detected on screening,” the Wadhwa team wrote.
Predicting axillary nodal status is important for staging and treatment planning for breast cancer patients. However, axillary node enlargement can occur with other metastatic cancers like melanoma, renal cell cancer, and lung cancer to name a few. Furthermore, benign unilateral axillary adenopathy can occur when the nodes react to ipsilateral vaccine administration, infection or trauma, tattoo pigment, or nonspecific etiologies.
This is where sonography comes into play. Breast imagers have used various sonographics to categorize benign versus malignant lymph nodes. These include size, shape, and morphologic features of the nodes. However, the researchers noted that it is “extremely difficult” to differentiate between malignant and benign lymphadenopathy on imaging, with biopsy often needed to confirm findings.
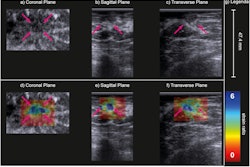
Wadhwa and colleagues sought to assess morphologic features of axillary nodes on ultrasound in predicting malignancy. They also wanted to explore the incidence of malignancy in axillary nodes based on their imaging mode of detection.
The team included data from 224 malignancies detected in 594 women who underwent an axillary node biopsy.
The authors noted that PPV was significantly associated with the extent of nodal cortical thickening (p < 0.0001). Nodes with cortical thickening of 5 mm or greater had the highest malignancy rate. The group found that 170 of the 308 nodes with such cortical thickening were malignant (55.2%). Additionally, breast cancer was the most common malignancy in each cortical thickening category, representing 80.8% in mild, 78.6% in moderate, and 60.6% in the significant category.
The researcher also found that the PPV of malignancy was significantly higher in nodes that lacked a normal hilum, a lymph vessel that directs lymph out of the node at the hollow side of the node. The PPV here was 61% for an abnormal hilum and 22% for a normal hilum.
The team also found that the PPV of malignancy in nodes detected on screening mammography or MRI was significantly lower than those detected by diagnostic imaging, palpation, or CT/PET.
| PPV of malignancy in nodes detected by modality | |||||
|---|---|---|---|---|---|
| MRI | Mammography | Palpation | Diagnostic imaging | PET/CT | |
| PPV | 15.8% | 18.8% | 43.8% | 48.4% | 65.3% |
| *Palpation, diagnostic imaging, and PET/CT achieved statistical significance compared with MRI and mammography. | |||||
Finally, the researchers found that of all screening-detected nodes in patients with no history of malignancy and mild cortical thickening, only two (4.3%) had malignancy.
“We propose that although the radiologists should keep a lower threshold for biopsy recommendation in patient with known cancer due to risk of micro-metastasis, the threshold should be higher in incidentally detected axillary adenopathy to decrease false positives,” the study authors wrote.
They also called for future studies on incidentally detected axillary lymphadenopathy, writing that this could help establish better guidelines for identifying abnormal nodes in this population.
The full study can be found here.