Lung ultrasound (LUS) scoring is reliable for determining whether preterm newborns need surfactant for suspected respiratory distress syndrome (RDS), a study published February 19 in Pediatrics & Neonatology found.
Researchers led by Shivendra Rai, MD, from King George’s Medical University in Lucknow, Uttar Pradesh, India, found that LUS scoring predicts surfactant administration better than chest x-ray in preterm neonates of 34 weeks' gestation admitted within 12 hours of birth with clinical suspicion of RDS.
“Based on interpreting artifacts that depend on the proportion of air and fluid in the lungs, various patterns are observed, and data indicate that it [LUS] is useful in managing RDS,” Rai and co-authors wrote.
Chest x-ray is used to diagnose RDS, but LUS has emerged as a reliable bedside tool for monitoring respiratory conditions in preterm infants. The researchers highlighted LUS as being noninvasive, nonionizing, and low cost, along with achieving high accuracy and being reliable and repeatable.
The Rai team studied the utility of LUS for preterm newborns at 34 weeks or less gestation admitted within 12 hours of birth with clinical suspicion of RDS. It also compared ultrasound scores with chest x-ray scores to predict the need for surfactant administration.
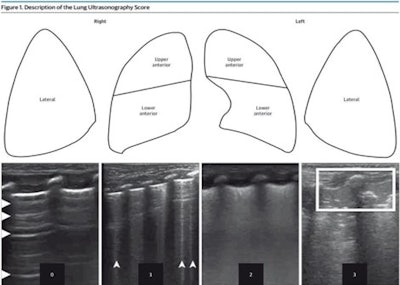 1Each lung has been split into three parts. Each area has been given a score between 0 and 3. Score values are shown in Ultrasonograms to match 4 different patterns. During a longitudinal scan with a high-resolution linear probe, pictures of patterns were taken. The scores are as follows: 0 means A pattern, 1 means B pattern, 2 means severe B pattern, and 3 means extended consolidation. Images available for publishing under a creative commons license, CC BY-NC-ND 4.0.
1Each lung has been split into three parts. Each area has been given a score between 0 and 3. Score values are shown in Ultrasonograms to match 4 different patterns. During a longitudinal scan with a high-resolution linear probe, pictures of patterns were taken. The scores are as follows: 0 means A pattern, 1 means B pattern, 2 means severe B pattern, and 3 means extended consolidation. Images available for publishing under a creative commons license, CC BY-NC-ND 4.0.
The prospective study included 67 preterm newborns admitted to the neonatal intensive care unit (NICU). They underwent a clinical exam, followed by a chest x-ray and LUS. Clinicians decided to administer surfactant based on the clinical picture and chest x-ray. The NICU team was blinded to LUS findings while the radiologist was blinded to the x-ray chest report.
Of the total newborns, 67.2% needed surfactant administration.
LUS scoring achieved a higher area under the curve (AUC) than that of the x-ray scoring, along with higher sensitivity and specificity.
| Comparison of LUS to x-ray scoring to determine whether preterm newborns need surfactant for suspected RDS | ||
|---|---|---|
| Measure | X-ray | LUS |
| AUC | 0.811 | 0.962 |
| Sensitivity | 93.3% | 95.6% |
| Specificity | 50% | 91% |
| Diagnostic accuracy | 80.1% | 88.1% |
The median LUS score was 12 among newborns who needed surfactant, while it was eight for newborns who did not need surfactant, the researchers reported. (LUS scoring ranges from 0 to 18.)
The study authors highlighted that their research “emphatically affirms” that LUS is a dependable tool in managing preterm newborns with RDS in low- and middle-income countries.
“This invaluable insight, well-established in neonatal units of developed nations, has now been substantiated by our study in the context of developing countries,” they wrote.
The authors also called for more studies on neonates receiving serial LUS during hospitalization.
The full study can be found here.