MRI and ultrasound have tradeoffs in diagnosing peripheral neuropathies of the upper extremity, a study published March 4 in Radiology found.
A team led by Daniel Schwarz, MD, from Heidelberg University Hospital in Germany found that MR neurography (MRN) has a higher accuracy and sensitivity while high-resolution nerve ultrasound (HRUS) achieved a higher specificity.
“This [MRN] may be the preferred imaging method when available, particularly for the suspected involvement of proximal nerve segments or multiple nerves,” the Schwarz team wrote.
High-resolution imaging provides important pathomorphological information in diagnosing peripheral nerve disorders. However, the researchers noted that the diagnostic role of such imaging remains unclear due to limited clinical evidence.
MRN and HRUS are two imaging techniques that have shown promise in this area. While HRUS provides high spatial resolution and is more cost-effective, MRN has “excellent” soft tissue contrast for both deep and superficial nerves and provides information about surrounding structures.
Schwarz and colleagues studied the diagnostic performance of both modalities in diagnosing peripheral neuropathies of the upper extremity, which is becoming more prevalent among the general population.
The prospective single-center study included 800 patients referred for clinically suspected peripheral neuropathy of the upper extremity. They were referred from 2015 to 2022. All patients underwent both HRUS and MRN, performed and interpreted independently by experienced neuroradiologists.
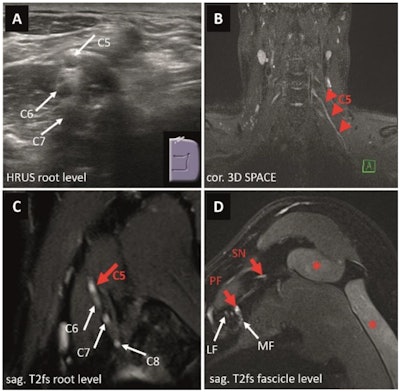 Images depict a 24-year-old male patient presenting with recurrent and exacerbating pain of his right shoulder with a difficulty to elevate (MRC 4+) his arm following a sports-related injury one year prior to imaging to rule out suspected plexus neuritis. On electrophysiology, only a borderline spontaneous activity pattern of the infraspinatus muscle was reported. On HRUS (A), the appearance of the supraclavicular plexus (dotted white line) was normal without suspicious alterations of nerve echogenicity or diameter. MRN of the proximal brachial plexus (B) suggested a possibly pathological T2 weighted signal increase at the conjunction of the inferior trunk (red dotted line) next to the unremarkable superior and middle trunk. However, there were no related clinical or electrophysiological findings. (C) Appearance of the distal, infraclavicular plexus segments including the lateral, medial, and posterior fascicles was normal as well as the suprascapular nerve. (D) No signs of muscular denervation of the supra- or infraspinatus muscles (*) were present on MRN. Therefore, a plexus neuritis or another nerve-related etiology was ruled out. An artificial signal increase, often caused by the magic-angle artifact, can lead to false-positive results on MRN and must be taken into consideration when interpreting MRN examinations. Images and caption courtesy of the RSNA.
Images depict a 24-year-old male patient presenting with recurrent and exacerbating pain of his right shoulder with a difficulty to elevate (MRC 4+) his arm following a sports-related injury one year prior to imaging to rule out suspected plexus neuritis. On electrophysiology, only a borderline spontaneous activity pattern of the infraspinatus muscle was reported. On HRUS (A), the appearance of the supraclavicular plexus (dotted white line) was normal without suspicious alterations of nerve echogenicity or diameter. MRN of the proximal brachial plexus (B) suggested a possibly pathological T2 weighted signal increase at the conjunction of the inferior trunk (red dotted line) next to the unremarkable superior and middle trunk. However, there were no related clinical or electrophysiological findings. (C) Appearance of the distal, infraclavicular plexus segments including the lateral, medial, and posterior fascicles was normal as well as the suprascapular nerve. (D) No signs of muscular denervation of the supra- or infraspinatus muscles (*) were present on MRN. Therefore, a plexus neuritis or another nerve-related etiology was ruled out. An artificial signal increase, often caused by the magic-angle artifact, can lead to false-positive results on MRN and must be taken into consideration when interpreting MRN examinations. Images and caption courtesy of the RSNA.
Both modalities had their share of tradeoffs in correctly diagnosing peripheral neuropathy.
| Performance comparison between MRN, HRUS | |||
|---|---|---|---|
| Measure | MRN | HRUS | p-value |
| Accuracy | 85.4% | 70.6% | < 0.001 |
| Sensitivity | 91.6% | 68.7% | < 0.001 |
| Specificity | 66.2% | 76% | < 0.001 |
On univariate analysis, the team reported that MRN sensitivity was significantly higher in the following cases: involvement of more than one nerve, proximal nerve involvement, lesion extent of more than two regions, or abnormal electrophysiology studies. MRN meanwhile was higher in cases of normal electrophysiology studies, no prior surgery, and in female patients.
And HRUS achieved significantly higher sensitivity in cases of peripheral nerve involvement, lesion extent of more than two regions, prior surgery, presence of sensory deficits, and abnormal electrophysiology studies. But HRUS specificity was higher in cases with normal electrophysiology exams, female patients, and no prior surgery.
With these results and comparable results observed in previous reports, the researchers wrote that MRN’s high sensitivity and accuracy over time “likely reflect the rapid technological advances and thus its increasing diagnostic potential.”
Despite the results, the study authors highlighted HRUS’ value as an adjunct tool or an alternative when MRN is not available or feasible. They added that advanced techniques such as ultra-high resolution, elastography, or assessment of intraneural blood flow could provide more tissue-specific information.
In an accompanying editorial, Swati Deshmukh, MD, from NYU Langone Health in New York City wrote that while more research is needed to confirm the roles of both modalities, they add to the potential value of advanced nerve imaging in diagnosing and assessing peripheral neuropathy as a non-invasive adjunct to clinical evaluation and electrophysiology.
"As imaging technology continues to improve, the interest in and demand for peripheral nerve imaging is growing," Deshmukh wrote. "Radiologist consultation regarding modality choice and technique will optimize peripheral nerve imaging and contribute to enhanced collaborative patient care."
The full study can be accessed here.




















