AI-guided point-of-care ultrasound (POCUS) can accurately detect tuberculosis (TB), according to research presented April 14 at the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) conference in Vienna, Austria.
In her presentation, Véronique Suttels, PhD, from Lausanne University Hospital in Switzerland discussed her team’s findings, showing that AI POCUS interpretation fulfills requirements by the World Health Organization (WHO) for a nonsputum TB triage test. The technology may have applications in clinically underserved areas, Suttels said.
“The AI algorithm easily surpassed the human expert interpretation,” she told AuntMinnie. “We gained in specificity when using AI algorithms to interpret these ultrasound images.”
Despite being treatable and preventable, pulmonary TB is still a global health challenge. TB rates rose by 4.6% from 2020 to 2023, according to a WHO report. Patients in vulnerable areas that don’t have easy access to clinical services are more likely to develop the disease. Suttels said that these inefficiencies worsen treatment delays and disease transmission.
 Véronique Suttels, PhD, performs an ultrasound scan on a patient in Benin, West Africa, using a POCUS scanner connected to a smartphone. Her team studied how an AI-guided POCUS system can help diagnose tuberculosis in patients with respiratory symptoms. Image courtesy of Véronique Suttels, PhD.
Véronique Suttels, PhD, performs an ultrasound scan on a patient in Benin, West Africa, using a POCUS scanner connected to a smartphone. Her team studied how an AI-guided POCUS system can help diagnose tuberculosis in patients with respiratory symptoms. Image courtesy of Véronique Suttels, PhD.
Researchers in imaging continue to explore ways that AI can benefit patients in these areas, with POCUS showing its potential in remote locations. Suttels highlighted lung POCUS being connected to a smartphone to make diagnoses and being sputum-free.
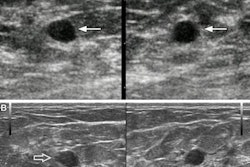
She and colleagues developed a suite of deep-learning (DL) models to automate TB risk assessment from lung ultrasound images. They named this suite ULTR-AI and it consists of the following: ULTR-AI, a DL model predicting TB directly from images; ULTR-AI[signs], which detects lung ultrasound signs as interpreted by readers; and ULTR-AI[max], which uses the highest risk score from both models.
The team conducted its study at a tertiary urban center in Benin, West Africa. Sonographers performed a standardized 14-point lung ultrasound sliding scan protocol. Human experts interpreted the images based on typical lung ultrasound findings.
The team compared the performances of these models with that of human experts who used a similar machine learning model.
Final analysis included 504 patients, 192 of whom had confirmed pulmonary TB. Also, 13% had a history of the disease and 15% were HIV-positive, with a median CD4 count of 92 cells/mm³ (IQR 43-358).
Among confirmed TB cases, 43% were underweight (body mass index < 18.5 kg/m²), 31% had a high quick organ failure score, 18% were hospitalized by day 28, and 3% died within that period.
The combined model, ULTR-AI[max], achieved a sensitivity of 91% and 85% specificity, as well as an area under the receiver operating characteristic curve of 0.93. This outperformed the human experts by 9%. It also exceeded the WHO’s thresholds of 90% sensitivity and 70% specificity for nonsputum-based tuberculosis triage tests.
Suttels said that through point-of-care TB triaging with minimal infrastructure and expertise, ULTR-AI could decentralize diagnostics in lower- to middle-income countries. This, in turn, would improve triaging for early detection and treatment, Suttels added.
“The end users for this tool, we envision, would be [practitioners] in all areas that do not have chest x-ray or primary healthcare centers that do not have a gene expert or need to send patients far away to get genetic tests to confirm TB suspicions,” she told AuntMinnie.com.
Suttels called for further validation in diverse populations to confirm the broader clinical utility of AI POCUS. She said the team plans to expand the use of their AI tools to more remote parts of Benin, Mali, and South Africa.